Six Paths Forward in Biomedical Research
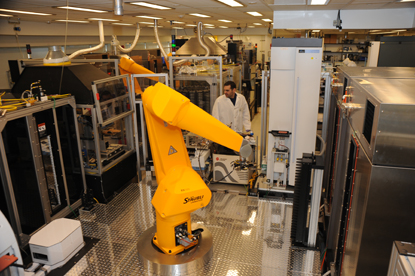
A high-throughput robotic screening system at NIH tests hundreds-of-thousands of compounds for their potentials to treat diseases.
Last month I moderated our annual retreat with the NIH Scientific Directors, those individuals tasked with leading their Institute or Center (IC)-based intramural research program. We were joined by many of the IC Clinical Directors. And this year we decided to do something a little different: listen to a series of talks about exciting, new IRP research.
In past years we focused on purely administrative matters, and that’s certainly important. In fact, our efforts in previous years in shaping long-term planning for the IRP — discussions of hires, space, equipment, and, of course, budgeting — have led us to this point we find ourselves now in which we contemplate ways to implement the areas of scientific emphasis that we enumerated in our long-term plan.
We discussed six research areas ripe for development: inflammatory diseases; genotyping and phenotyping; cell-based therapies; neuroscience and compulsive disorders; RNA biology and therapeutics; and the microbiome. More than just a string of hot science topics, these are areas in which the IRP is uniquely positioned to excel and become a prime destination, helping to secure our relevance in the decades to come.

The C.W. Bill Young Center for Biodefense and Emerging Infectious Diseases
Inflammatory diseases
We heard presentations from Danny Reich on multiple sclerosis (MS) and Tom Wynn on chronic fibrotic diseases. The connection? Many fields once considered disparate are now seen as interconnected, such as innate immunity, metabolism, and the microbiome. It’s hard to think of a disease that doesn’t have an inflammatory element. MS now is seen as a chronic inflammatory disease, which may change treatment targets. Fibrosis is at the root of inflammation, marking that fine balance between tissue repair and the demise of organ function. At the NIH, we have both the tools and expertise at the basic science and clinical levels, coupled with mechanisms to collaborate with industry, to develop a new generation of therapies for inflammatory disease…and maybe tackle the ill effects of aging, which some see as the ultimate inflammatory disease.

The NIH Clinical Center
Genotyping & phenotyping
The IRP is without question a terrific place to develop predictive genomic medicine, providing deep phenotyping of individuals whose genotypes signal the possibility of unusual manifestations of disease or normal variants. We can tap into patient populations already genotyped at the NIH Clinical Center (CC), our massive and mature cohort studies, such as the Framingham Heart Study and NIEHS’ studies of genetic determinants of environmental response, and other local genotyping centers. These study participants are available for recall and long-term follow-up. At the SD retreat, Richard Siegel described a unique opportunity to engage CC patients, existing cohorts, and also blood and bone marrow donors for an unprecedented genotype/phenotype open database. In what is surely proof of concept, Josh Milner described monogenic causes for allergic diseases in which elevated alpha-tryptase levels are seen after anaphylaxis. His important discovery was possible because of the easy access to connected datasets: single nucleotide polymorphisms from Merck and the NIAID Clinical Exome Initiative, and high tryptase values from the CC Biomedical Translational Research Information System.
Cell-based therapies
Here’s another thoroughly trans-NIH opportunity. Steve Rosenberg’s immunotherapy work is among the highest-profile clinical advances in recent years. But it doesn’t stop there. At the SD retreat, Christian Hinrichs described adoptive T-cell therapies with initial successes in treating epithelial cell cancers, using HPV cancer as a model. (A flowchart to depict the hundreds of NIH basic research projects from the past four decades that made this work possible would be dizzying.) On the induced pluripotent stem cell (iPSC) front, Kapil Bharti described his promising clinical work on age-related macular degeneration. We have the diverse talent to lead in cell-based therapies. The only rate-determining step is the capacity for cell processing at the CC Division of Transfusion Medicine and the availability of Current Good Manufacturing Practice (cGMP) facilities, both of which we are actively addressing.

The John Edward Porter Neuroscience Research Center
Neuroscience and compulsive disorders
To paraphrase a slogan for higher education, mind research is a terrible thing to waste. Opportunities abound, and we are now focused on maximizing our investment in the Porter Neuroscience Center (Building 35), a collaborative venue housing neuroscientists from 10 ICs. At the SD retreat, Veronica Alvarez described neuronal properties and pathways underlying compulsive disorders. Think about it: almost all of us have some compulsive disorder, be it nail-biting or something more serious, and these disorders can manifest in health-compromising conditions, such as obesity or addiction. As a follow-up, postdoctoral fellow Michael Krashes described how stimulating AgRP expression in mice would make these animals eat even if they were already full and suppress their fears to get more food. We have a proposal on the table to create a center on compulsive disorders which could yield exciting discoveries.
RNA biology and therapeutics
Once again, we find ourselves needing to take better advantage of what we already have. The IRP is thick with RNA biologists, but are we not seeing the woods for the trees? Sandra Wolin, newly recruited as a CCR lab chief from Yale, where she directed the Yale Center for RNA Science and Medicine, outlined the need for a virtual center at NIH for RNA that would feature a director, a steering committee, a website, and an annual meeting or symposium to address the need for unifying the field and giving RNA a visible presence at the NIH. In an ironic evolutionary twist, RNA is the new DNA when it comes to therapeutic targets. As such, Adrian Ferre-D’Amare presented his findings about the “dark matter of the transcriptome” and discussed how RNA is “ancient, stiff, modular, highly evolvable, and stereochemically precise.” In short, the science is hard but the reward is sweet.
Microbiome
With apologies to John Donne, it turns out we are islands — islands on which untold species of bacteria, archaea, protists, fungi, viruses, and bacteriophages work, play, and live. Surprisingly, only recently are we realizing how important the microbiome is to human health. The wrong balance of island inhabitants on and in our bodies, and chronic disease can take hold. At the SD retreat, Yasmine Belkaid described her award-winning research on the skin microbiome and other work at the NIH in the past few years. And Giorgio Trinchieri discussed his new line of research on the connection of the microbiome to cancers. The field is intertwined with immunology.
So, that’s what’s on the table for discussion. I’m not saying these are the only areas to develop. Nevertheless, the SDs as well as I and my staff were enthralled by the presentations and the possibilities that confront us. Expect noticeable action by the end of this year in accelerating progress in at least some of these scientific themes.
Related Blog Posts
This page was last updated on Thursday, January 4, 2024
