Shaping Therapies for Sickle Cell Disease
Swee Lay Thein is hunting for new ways to help patients with deformed red blood cells.

On December 8, 2023, science fiction became reality when the U.S. Food and Drug Administration (FDA) approved a first-of-its-kind gene-editing therapy for sickle cell disease. But while the treatment could be life-changing, even the scientist whose work laid the foundation for it, Dr. Swee Lay Thein, acknowledges that gene editing won’t be an option any time soon for most of the 8 million people affected by the condition.
“These treatments require really good medical infrastructure and they cost two to three million dollars,” explains Dr. Thein, Chief of the Sickle Cell Branch at NIH’s National Heart, Lung, and Blood Institute (NHLBI). “Right now, it’s really beyond the reach of the vast majority of patients, even in developed and well-resourced countries.”
Instead, Dr. Thein is focused on finding new medications for sickle cell disease, which stems from mutations in both copies of the gene that produces red blood cells’ oxygen-carrying hemoglobin protein. When the abnormal protein is not carrying much oxygen, it causes the cells to stiffen and deform into the disease’s characteristic ‘sickle’ shape. As a result, the cells jam up blood vessels, cutting off the oxygen supply to parts of the body and causing incredibly painful episodes called ‘crises.’ Right now, doctors’ go-to for treating sickle cell disease is a medication called hydroxyurea, but it doesn’t entirely alleviate symptoms in some patients and causes side effects like constant nausea in others.
“Just like for high blood pressure, we need more than one drug because for some patients a certain drug might not work so well,” Dr. Thein says.
In 2007, while working at Kings College London in the United Kingdom, Dr. Thein was studying a gene called BCL11A, which usually turns on shortly after birth and stops the body from producing the form of hemoglobin that is made in a developing fetus. However, her research team discovered that sickle cell patients with certain BCL11A variants continued to produce that ‘fetal’ hemoglobin as adults. Their fetal hemoglobin significantly reduced their symptoms, and the new gene editing treatment works by inhibiting BCL11A in order to reawaken the body’s ability to make fetal hemoglobin. In 2024, that research earned Dr. Thein a share of the prestigious Shaw Prize in Life Science and Medicine.
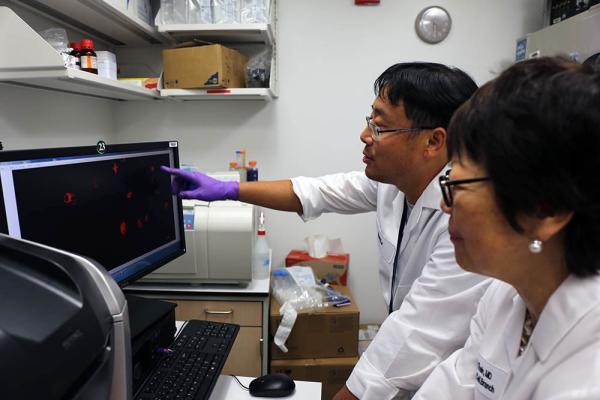
Staff scientist Kang Le and Dr. Thein examine immune cells called macrophages that have been exposed to the blood of patients with sickle cell disease. The experiment revealed that the patients’ blood caused damage to the immune cells’ DNA, revealing a key reason why patients with sickle cell disease experience noticeable inflammation throughout their bodies.
However, linking BCL11A to the production of fetal hemoglobin wasn’t the only important discovery Dr. Thein made at Kings College. Among the patients she treated there was a woman who had all the classic symptoms of sickle cell disease, yet had only one mutated hemoglobin gene, not the two typically needed to give rise to the condition. The patient’s other, normal copy of the gene should have produced normal hemoglobin and prevented any symptoms — a puzzle that confounded Dr. Thein.
The answer to this conundrum lay in yet another genetic mutation — this time in one copy of the patient’s PKLR gene, which compromised production of an enzyme called pyruvate kinase. Less pyruvate kinase, in turn, caused another enzyme called 2,3-DPG to build up in her red blood cells. Because 2,3-DPG reduces hemoglobin’s ability to bind oxygen, the combination of her one mutated hemoglobin gene and the excess 2,3-DPG in her red blood cells caused the cells to bend into the classic sickle shape.
“This made me think, ‘If you are deficient in pyruvate kinase and it makes sickle cell disease worse, what if you increase pyruvate kinase?’” Dr. Thein recalls. “Can you do the reverse?”
When she came to NIH to run the Sickle Cell Branch in 2015, Dr. Thein went hunting for a way to boost pyruvate kinase production and came across mitapivat, an experimental treatment for people who have mutations in both copies of the PKLR gene. Mitapivat eventually received FDA approval in 2022 for adults with that disease, known as pyruvate kinase deficiency, but a decade ago it was still experimental and the company that created it was not studying its applications to sickle cell disease. Dr. Thein convinced the company to let her give it a try.
The resulting clinical trial not only suggested mitapivat was safe for sickle cell patients, but also supported Dr. Thein’s hunch that turbo-charging pyruvate kinase production could help those individuals. The higher the dose of the medication patients in the trial received, the less of the deformation-inducing 2,3-DPG protein their red blood cells harbored. The treatment also appeared to make those cells less fragile, an effect of their sickle shape that can cause patients to become anemic if the cells break apart faster than the body can replace them. When Dr. Thein’s team examined why, they found that mitapivat altered the way red blood cells modify a different protein that helps them maintain their shape.
This video, produced by an experiment in Dr. Thein’s lab, shows that sickle red blood cells from patients with sickle cell disease have energy-generating mitochondria (green), which normal red blood cells do not — yet another abnormality Dr. Thein's research has revealed about the red blood cells of people with the condition.
“Normally, red blood cells can elongate, but sickle cells cannot elongate so well,” she explains. “That’s part of the problem — sickle cells are so deformed and inflexible that they cannot squeeze through fine blood vessels. We showed that when patients are on this treatment, their red cells’ elongation improves and they can squeeze through.”
The encouraging results of Dr. Thein’s clinical trial spurred the company developing mitaptivat to conduct another, larger study of its own, which also showed the drug’s promise for treating sickle cell disease. Dr. Thein’s team is now conducting a large phase 3 clinical trial of mitapivat at the NIH Clinical Center that began enrolling patients in May 2024, as well as a study tracking the long-term safety of the drug for sickle cell patients.

Lab manager Britney Kruah prepares DNA samples from patients with sickle cell disease for whole genome sequencing analysis.
Further probing the intricacies of the PKLR gene could also one day help doctors figure out the best way to treat sickle cell disease, whether with mitapivat or another drug. Dr. Thein’s IRP team has found that sickle cell patients with certain variations in that gene are more frequently hospitalized due to sickle cell crises, which suggests PKLR influences the severity of the condition’s symptoms. If that turns out to be true, examining sickle cell patients' PKLR genes might one day inform how high a dose of medication they should take.
“I find that doing science, in a lot of ways, is curiosity-driven — you find a lot of dots, and then eventually the dots start to connect,” Dr. Thein says.
She isn’t satisfied with just adding mitapivat to the list of sickle cell treatments, though. Her research group recently teamed up with the lab of IRP senior investigator Will Eaton, M.D., Ph.D., to examine how more than 12,600 medications — all of which are either already FDA-approved or are being tested in clinical trials — affected the sickle-like deformation of red blood cells. The study ultimately identified 21 drugs that might be useful for treating sickle cell disease — including, once again, mitapivat.
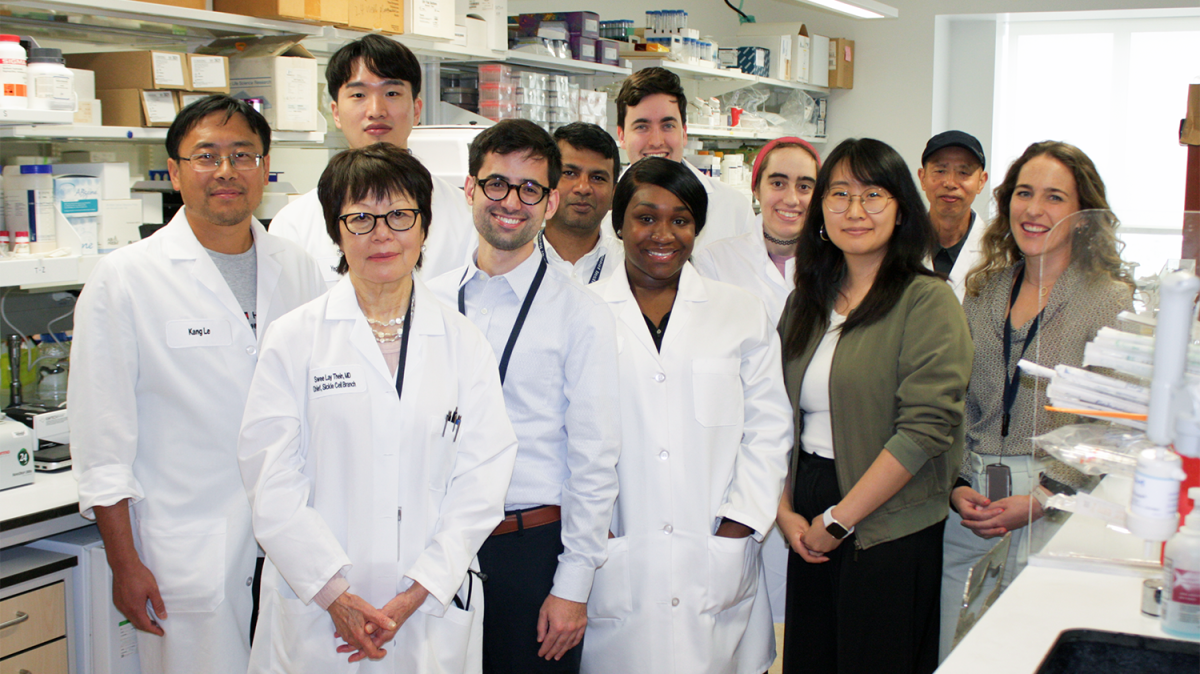
Dr. Thein’s lab staff. From left to right: staff scientist Kang Le, Dr. Thein, postbaccalaureate fellow Yechan Cho, staff clinician Sebastian Mendez Marti, postdoctoral fellow Rudra Ray, Lab Manager Britney Kruah, postbaccalaureate fellow Quinlan Batcheller, lab technician Kylie Haymaker, staff assistant Tiffany Chen, staff scientist Xunde Wang, and visiting postdoctoral researcher Eileen Ryan.
Meanwhile, Dr. Thein also hopes to one day discover a way to quickly end excruciating sickle cell crises. After nearly a decade at NIH, she has come to appreciate how working in the IRP facilitates the sort of bench-to-bedside research that could give rise to such a treatment.
“Never in my wildest dreams did I think I’d be able to come to the NIH,” she says. “It is really a great example of how clinical and translational research could and should be done.”
“Coming here gave me this opportunity to put what always intrigued me at Kings College into real practice,” she adds, “and now I'm really excited to find more medications for this patient population.”
Swee Lay Thein, F.R.C.P, D.Sc., is the Chief of the Sickle Cell Branch at the National Heart, Lung, and Blood Institute (NHLBI).
This page was last updated on Monday, September 9, 2024