IRP’s Cynthia Dunbar Elected to National Academy of Medicine
Studies of Blood Stem Cells Stimulate Pioneering Therapeutic Approaches

Dr. Cynthia Dunbar was elected to the National Academy of Medicine last year for her discoveries about critical blood-producing stem cells.
The National Academy of Medicine (NAM), first established in 1970 by the National Academy of Sciences as the Institute of Medicine (IOM), is comprised of more than 2,000 elected members from around the world who provide scientific and policy guidance on important matters relating to human health. Election to the NAM is considered one of the highest honors in the fields of health and medicine and recognizes individuals who have not only made critical scientific discoveries but have also demonstrated a laudable commitment to public service.
IRP Distinguished Investigator Cynthia E. Dunbar, M.D., was elected to the NAM last year for her pioneering research into hematopoietic stem cells, the cells in bone marrow that develop into oxygen-carrying red blood cells, infection-fighting white blood cells, and clot-forming platelets. Her work has led to valuable insights into the production of those blood cells, called hematopoiesis, and its role in human health. Her discoveries have also resulted in new approaches to treat disease by improving stem cell functioning or manipulating stem cells with gene therapy.
“I’m excited to be elected because it means my peers appreciate my contributions to science and clinical care throughout my career,” Dr. Dunbar says of her election to the NAM. “It’s also a nice stamp of quality approval for NIH’s Intramural Research Program.”
Growing up in Westport, Connecticut, Dr. Dunbar was always interested in science. During her sophomore year in high school, a close friend developed Hodgkin lymphoma, a cancer stemming from white blood cells called lymphocytes. She spent a lot of time visiting him at Yale-New Haven hospital while he underwent treatment, but he just missed benefiting from curative therapies that now make his cancer survivable, and he sadly passed away during their senior year. She decided then to pursue a career in medicine.
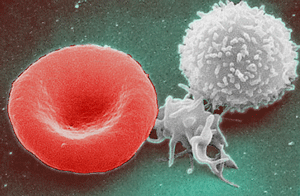
Hematopoietic stem cells develop into oxygen-carrying red blood cells (left), infection-fighting white blood cells (right), and clot-forming platelets (middle).
During medical school at Harvard University, Dr. Dunbar further developed her interest in hematology, the study of blood, and while completing a residency in Boston she applied to clinical fellowships in hematology-oncology to get training in treating cancers of the blood. Having majored in history as an undergraduate, she had little laboratory research experience at that point and expected to end up as a clinical investigator or practitioner. However, her career path took a turn when she applied to the medical oncology fellowship program at the NIH’s National Cancer Institute (NCI) without realizing there was no clinical hematology training available at the NIH at that time. What’s more, a box she checked on a confusing application form landed her in a group interview with several branch chiefs from the National Heart, Lung, and Blood Institute (NHLBI) for what turned out to be an extra year of residency.
“It became clear one minute into the interview that there was no way I needed or wanted to do an extra year of residency,” Dr. Dunbar remembers.

Former IRP investigator Arthur Nienhuis mentored Dr. Dunbar during her early years at the NIH.
Fortunately, some good did come out of the mix-up. One of the IRP branch chiefs in the room, Arthur Nienhuis, M.D., then head of the NHLBI’s Clinical Hematology Branch, was impressed by her and invited her to work in his lab as a clinical associate, stressing that she could acquire intensive training in laboratory research and explore that potential direction for her career. He was committed to providing this training to physicians, which he felt was critical to hematology due to the close connection between advances in molecular biology and progress in clinical practices. After three years in Dr. Nienhuis’ lab, Dr. Dunbar left for a year of official clinical fellowship training in hematology at the University of California, San Francisco, before returning to the NIH to set up her own research program in 1991.
Dr. Dunbar’s work focuses on understanding the basic properties of hematopoietic stem cells (HSCs): how many exist in the human body; how long each HSC keeps functioning and whether they can be ‘exhausted;’ what happens to HSCs during aging; and what events contribute to disease-causing HSC abnormalities. Answering these questions could lead to improved treatments for patients in which HSCs fail to properly produce blood cells. Such malfunctions can lead to a lack of red blood cells, known as anemia; an increased risk of infection; or bone marrow and immune system cancers like the one that led to the death of her friend in high school.
“Stem cell biology always seems to lead the way in science,” Dr. Dunbar says, possibly because blood and bone marrow cells are so easy to obtain and study in the laboratory.
More From the IRP
Podcast
Dr. Cynthia Dunbar — Stem Cell Therapies for Blood and Immune System Diseases
Using tools like the polymerase chain reaction (PCR) and whole genome sequencing, scientists like Dr. Dunbar have made huge leaps in their understanding of stem cells and how to manipulate them. In the future, scientists may even be able to correct abnormal genes in HSCs to permanently reverse disorders like sickle cell disease, which creates dysfunctional, misshapen red blood cells.
“The more we understand hematopoietic stem cells, the better we’re getting at genetically modifying them and having gene therapies work,” Dr. Dunbar says.
Recently, Dr. Dunbar’s focus has turned to what happens when HSCs age and whether that might explain why older individuals are at increased risk for certain cancers and other blood-related illnesses. Her research team has also found that abnormalities that arise in stem cells as people age may contribute to an increased risk of heart disease and even the inflammatory response seen in some patients with COVID-19.

Dr. Cynthia Dunbar and her IRP colleague Dr. Neal Young showed that a drug called eltrombopag, which stimulates hematopoietic stem cells in the bone marrow to produce more blood cells, provides noticeable benefits to patients with aplastic anemia.
While much of Dr. Dunbar’s work focuses on basic science, she is actively involved in clinical trials as well. For instance, she teamed up with fellow IRP senior investigator Neal Young, M.D., on a clinical trial for severe aplastic anemia, a bone marrow disease in which the body creates too few blood cells of all types. Until that trial, patients with the condition were primarily treated with repeated blood transfusions and drugs that suppress the immune system, which come with significant risks of their own. Together, Drs. Dunbar and Young showed that a drug called eltrombopag, which stimulates HSCs to ramp up production of blood cells with few side effects, provided noticeable benefits for very ill patients who had had little success with other treatments. Following the trial, eltrombopag was approved by the FDA as a treatment for various stages of asplastic anemia in 2014 and 2017 and became the standard of care for the disease.
Alongside her research, sharing her expertise and mentoring up-and-coming physicians and scientists remains central to Dr. Dunbar’s mission. When she returned to the NIH in 1991 after her year away, one of the first things she did was set up a hematology fellowship program so that IRP trainees would not have to go elsewhere, as she did, to finish their clinical educations in hematology. She directed that program for 17 years before stepping down in 2008.

Dr. Dunbar examines cells under a microscope.
As the first female editor of the American Society for Hematology’s premier journal, Blood, Dr. Dunbar considers it particularly important to support women in science. She is active in a program called Executive Leadership for Academic Medicine, which helps train women to be leaders at academic centers around the country. Additionally, in 2005, Dr. Dunbar and Dr. Zeke Emanuel, chair of the Bioethics Department at the NIH Clinical Center, revived the NIH Assembly of Scientists to advise NIH leadership and represent the concerns of NIH’s scientific and clinical staff in top-level decision-making. She is very active in a committee aimed at ensuring equity for female researchers and those from groups under-represented in the sciences.
“You can't just complain about things,” Dr. Dunbar says. “You have to try to fix them.”
Joining the NAM will give Dr. Dunbar another opportunity to advocate for science and scientists.
“The NAM’s mission is a very important one in terms of convening experts to give unbiased advice to government agencies and other bodies trying to decide what to do about complex problems in health,” Dr. Dunbar says. “It's exciting to participate in those committees as an actual member of the Academy.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
Related Blog Posts
This page was last updated on Monday, January 29, 2024
