Saving the Skin From a Renegade Immune Reaction
IRP Study Provides Insight into Cancer Treatment’s Skin-Thickening Side Effects

New IRP research could eventually improve treatment for cancer patients and others who experience skin problems after receiving a transplant of the body’s blood-producing ‘hematopoietic’ stem cells.
Scientists have long dreamt of leveraging information about our genes to personalize medical treatment. However, in working towards that effort, they have increasingly discovered the importance not just of what genetic variants are present in a person’s DNA, but how active each of those genes is. Now, new IRP research suggests the possibility of using that information to personalize medical treatment for patients who experience serious skin problems after receiving a transplant of the bone marrow’s blood-producing stem cells.1
Certain genetic conditions, as well as cancers like leukemia that affect the blood, are often treated with hematopoietic stem cell transplants, which replace the blood-producing ‘hematopoietic’ stem cells in a patient’s bone marrow with those of another individual. Since those cells are responsible for producing all the body’s immune cells, the procedure is akin to a complete immune system reboot. Unfortunately, those new immune cells don’t always play nice with the recipient’s body, leading to a life-threatening condition called ‘graft versus host disease.’
“When people develop graft versus host disease in the skin, it can take many different forms, and that’s one of the challenges of treating the disease,” says IRP senior clinician Edward Cowen, M.D., the new study’s senior author. “In patients who have the form of the disease where the skin and its underlying tissues thicken, that makes the skin less pliable and the joints less moveable. Depending on where you have it in the body, it can even make it harder to breathe because you have to move the skin around the ribs and diaphragm area in order to take a deep breath. It can be quite debilitating and painful, and even if it doesn’t directly lead to a patient’s death, it can significantly affect their quality of life.”
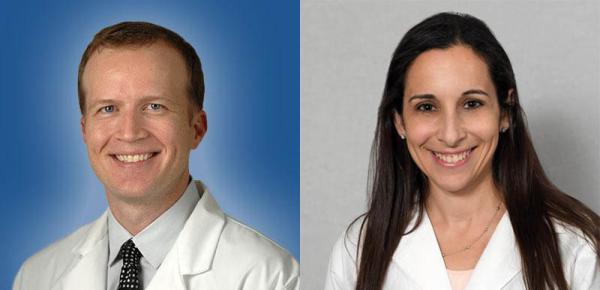
The new study was led by Dr. Cowen (left) and former IRP research fellow Rachel Rosenstein (right), who is now an assistant professor at Hackensack Meridian School of Medicine in New Jersey.
In the new study, former IRP research fellow Rachel Rosenstein M.D., Ph.D., the paper’s first author, worked with Dr. Cowen and other IRP scientists to drill down to the root cause of that complication, which affects roughly 10 percent of patients who have long-lasting graft versus host symptoms. To do so, they collected skin and blood samples from recipients of hematopoietic stem cell transplants who experienced that side effect and compared them to samples from transplant recipients who had not.
Skin cells from all the patients with post-transplant skin thickening showed substantially greater activity in several genes related to a process called fibrosis, in which a structural protein called collagen — the main protein found in scar tissue — gets deposited in areas of the body. Genes related to inflammation were also over-active, on average, in those patients’ skin compared to those without skin thickening. However, further analysis revealed that only a subset of patients with post-transplant skin thickening had inflammatory genes that were stuck in overdrive, while the rest had fairly typical levels of activity in those genes.
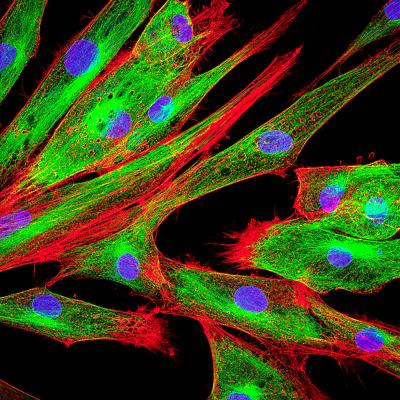
Cells called fibroblasts, pictured here, are responsible for fibrosis. Graft versus host disease appears to boost how active they are in some patients’ skin.
“It’s thought that the fibrosis is triggered by inflammation, but we’re seeing that a lot of these patients have fibrosis without inflammation,” explains Dr. Rosenstein, who is now an assistant professor at Hackensack Meridian School of Medicine in New Jersey. “It’s likely that inflammation initially stimulated this response, but either it has calmed down on its own or the medications patients are on have suppressed the inflammation, yet they still continue to have fibrosis.”
“It suggests that perhaps a better way to treat those patients without a lot of inflammation would be to target more of the fibrotic pathways, which typically are not targeted by the current approved treatments for graft versus host that predominantly target inflammation,” she adds.
After analyzing gene activity in the participants’ skin, the IRP researchers selected several genes that were over-active in the skin of graft versus host patients with skin thickening and measured the amounts of the genes’ corresponding proteins in the participants’ blood. This analysis revealed three proteins — SFRP4, SERPINE2, and COMP — that were more abundant in the blood of those patients than in the blood of patients without skin thickening. This difference was noticeable even though some of the patients without skin thickening were experiencing graft versus host symptoms affecting parts of the body other than the skin, suggesting that those three proteins might be specifically involved in graft versus host’s effects on the skin.

The new study’s results suggest that doctors may one day be able to use a simple blood test to identify patients likely to experience symptoms of graft versus host disease in their skin.
The identification of biomarkers like those three proteins could give clinicians a more objective and sensitive way to gauge the behavior of biological systems responsible for skin thickening in patients with graft versus host disease. That, in turn, could speed up clinical trials of treatments for those patients, as well as help doctors more quickly identify patients likely to experience skin problems after hematopoietic stem cell transplants so they can intervene earlier and potentially stave off serious symptoms. Meanwhile, the knowledge that some patients experience skin thickening after their transplants despite low levels of inflammation in their skin could help doctors tailor treatment decisions, perhaps leading them to prescribe drugs that target fibrosis-related biological pathways while lowering doses of ‘immunosuppressive’ medications that treat inflammation by broadly hampering the immune system.
“If we can find a tissue biomarker — something that gives a readout of the need to target fibrosis versus inflammation — then that’s one step closer to individualized therapy as opposed to using less specific immunosuppressive drugs, which is the standard,” Dr. Cowen says. “For most people who die after a transplant, if they don’t die from a recurrence of their cancer, they usually die from infection. Our immunosuppressive treatments put them at higher risk for that, so we want to find better treatments that directly target the cause, whether it’s inflammation or fibrosis.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Rosenstein RK, Rose JJ, Brooks SR, Tsai WL, Gadina M, Pavletic SZ, Nagao K, Cowen EW. Identification of Fibroinflammatory and Fibrotic Transcriptomic Subsets of Human Cutaneous Sclerotic Chronic Graft-Versus-Host Disease. JID Innov. 2023 Dec 7;4(2):100246. doi: 10.1016/j.xjidi.2023.100246.
Related Blog Posts
This page was last updated on Tuesday, April 9, 2024
