A New Model of an Old Itch
IRP’s Marc Ferrer Grows 3D Skin to Study Eczema

IRP researchers hope to speed the development of new treatments for the skin condition known as eczema by printing realistic models of human skin in the lab.
Traditional ways of assessing the effectiveness and safety of potential new drugs don’t exactly mimic the human body. After all, we are not jumbo-sized mice, nor are we flat swaths of a single type of cell spread across a petri dish. As a result, many drugs that initially show promising results when tested on cell or animal models turn out to be disappointing in clinical trials.
That’s why scientists like the IRP’s Marc Ferrer, Ph.D., are developing more realistic models of human tissues, which give a more accurate picture of how well a drug might work in people. As we observe Eczema Awareness Month in October, we spoke with Dr. Ferrer, Director of NIH’s 3D Tissue Bioprinting Laboratory, about the efforts of his group to create a better model of human skin for testing treatments for that condition, which causes dry, itchy skin for more than 30 million Americans.
“We’re very interested in what’s called ‘non-animal models,’ including 3D tissue models,” Dr. Ferrer says. “Currently, scientists are using cells grown on plastic that are totally outside the human context. As a result, we get beautiful responses from compounds being developed as potential drugs, but they don’t translate into what happens in humans.”
By assembling tissue models — that is, putting human cells in a dish in a way that more closely resembles real human tissue — the hope is that cells will respond to potential drugs in a way that is closer to what happens inside a real person. For this particular project, Dr. Ferrer’s team recreated skin tissue, complete with the different layers found in human skin, by using a 3D ‘bioprinter,’ a machine that can print human cells in three dimensions in the same way a normal printer uses ink.

Kristy Derr-Mierzwa, a research scientist in Dr. Ferrer’s lab, shows off the 3D bioprinter Dr. Ferrer’s team uses to make 3D skin tissue models.
Dr. Ferrer’s lab began working on making the skin tissue models when it acquired its 3D bioprinting machine, eager to make use of the new tool.
“At the beginning, we were looking for tissue models that we could use to learn how to use the technology, which was new for us,” he recalls. “We thought skin would be a good model because the technology is particularly good for tissue with layers.”
One key reason that Dr. Ferrer’s team can create realistic skin tissue is that the 3D bioprinting process can mimic the events that skin cells called keratinocytes experience in real human skin. Those cells, which make up 90 percent of the skin’s outermost layer, begin life under the skin’s surface and rise to its exterior over time, changing their characteristics and gaining new abilities along the way. Finally, exposure to air at the skin’s surface triggers the final stages of their life cycle. The same process occurs when keratinocytes are exposed to air in the tissue models Dr. Ferrer’s team creates with its bioprinter. As a result, Dr. Ferrer’s team can create skin tissue with the complexity of real skin, including blood vessels and multiple layers. They then place these tiny sheets of artificial skin into dishes with multiple deep wells, sort of like very tiny muffin tins, that have space for the different layers.
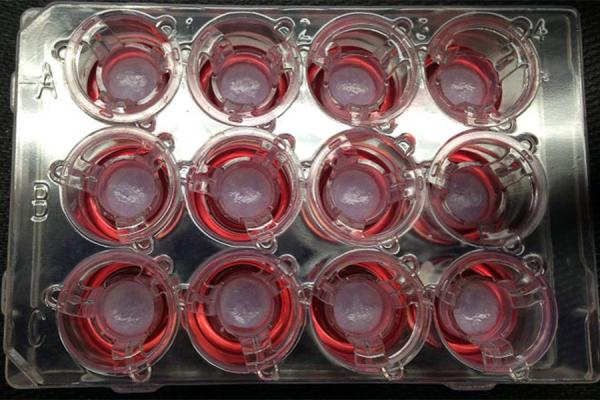
The artificial skin produced in Dr. Ferrer’s lab spends its life in dishes like this one.
Once Dr. Ferrer’s team managed to create realistic skin tissue in the lab, it looked for opportunities to use it to study skin diseases, so they decided to try creating a model of eczema. Since eczema involves an immune system reaction that changes the way keratinocytes behave, Dr. Ferrer’s team uses its 3D tissue models to examine how those cells react to specific molecules released by the immune system. The group began by reproducing the acute stage of the illness, in which immune cells secrete a molecule called interleukin 4, or IL-4. 2
“It’s very difficult to reproduce the disease from beginning to end, so we broke it down into different stages,” Dr. Ferrer explains. “We added IL-4 to our 3D skin models to see if they would reproduce the lesions or rash you see in eczema, and we found that they did indeed look like the ones you see in human eczema.”
The next step was to see if they could use these same tissue models to find new drugs that might be more effective in treating the disease. The IRP research team did this by examining whether a type of medication already used to treat eczema, called a JAK inhibitor, could reverse signs of eczema in the model. The technique worked, establishing the model as a promising means of evaluating new drug candidates for their effects on eczema.3
Now, Dr. Ferrer’s research team is working with groups within NIH4 and at academic medical centers around the country to develop similar 3D tissue models that can be used to test potential treatments for other skin ailments, including psoriasis, viral skin infections, and skin cancers.

Dr. Marc Ferrer
“We're trying to demonstrate that we can develop disease models and use them to generate data that is actually useful for taking a drug from preclinical testing through to an investigational new drug application,” Dr. Ferrer says. “I think the dream is that, eventually, these models will be sufficient to show not only a drug’s efficacy in reversing a disease’s effects, but also its safety and potential toxicity.”
Ultimately, Dr. Ferrer hopes this technique can be taken even further by including immune cells so that the models can reflect the immune system’s role in certain diseases affecting the skin, as well as by harnessing artificial intelligence and machine learning to help scientists better predict how potential new drugs will affect humans. His approach may also prove to be a particular boon for the study of very rare diseases by allowing scientists to essentially grow a life-like version of a single patient’s skin in the lab.
“I think it's very exciting work,” Dr. Ferrer says. “We need to work together as a biomedical community in a pre-competitive space to assess how useful these tissue models are to developing better treatments for patients. There's a lot of work now being done in this area, and I really have high hopes that now we will make an impact.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Jung O, Song MJ, Ferrer M. Operationalizing the use of biofabricated tissue models as preclinical screening platforms for drug discovery and development.(external link) SLAS Discov. 2021. 26(9):1164-1176. doi: 10.1177/24725552211030903.
[2] Liu X, Michael S, Bharti K, Ferrer M, Song MJ. A biofabricated vascularized skin model of atopic dermatitis for preclinical studies. Biofabrication. 2020. 12(3):035002. doi: 10.1088/1758-5090/ab76a1.
[3] Wei Z, Liu X, Ooka M, Zhang L, Song MJ, Huang R, Kleinstreuer NC, Simeonov A, Xia M, Ferrer M. Two-dimensional cellular and three-dimensional bio-printed skin models to screen topical-use compounds for irritation potential. Front Bioeng Biotechnol. 2020. 8:109. doi: 10.3389/fbioe.2020.00109.
[4] Myles IA, Castillo CR, Barbian KD, Kanakabandi K, Virtaneva K, Fitzmeyer E, Paneru M, Otaizo-Carrasquero F, Myers TG, Markowitz TE, Moore IN, Liu X, Ferrer M, Sakamachi Y, Garantziotis S, Swamydas M, Lionakis MS, Anderson ED, Earland NJ, Ganesan S, Sun AA, Bergerson JRE, Silverman RA, Petersen M, Martens CA, & Datta SK. 2020. Therapeutic responses to Roseomonas mucosa in atopic dermatitis may involve lipid-mediated TNF-related epithelial repair. Sci. Transl. Med. 12(560):eaaz8631. doi: 10.1126/scitranslmed.aaz8631.
Related Blog Posts
This page was last updated on Wednesday, October 11, 2023
