Pandemic Brings All Hands on Deck
IRP Investigators Begin Hundreds of New Coronavirus-Related Studies
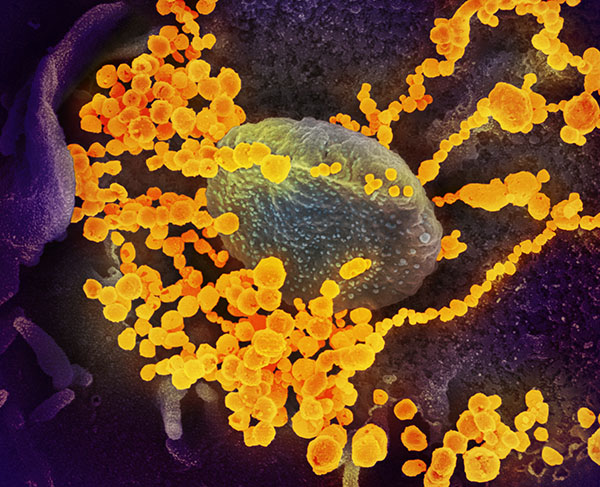
Just like the novel coronavirus swarms our cells, a wave of IRP researchers is contributing to efforts to learn more about the highly contagious illness.
Within just a few months after COVID-19 began spreading in the United States, IRP researchers had already made numerous important contributions to the fight against the deadly virus. Scientific knowledge about the disease continues to expand at a unprecedented pace, and the IRP will continue to play a major role in this effort over the coming months and years. In fact, nearly 300 new intramural research projects related to the novel coronavirus are currently starting up or have already begun.
Investigators across the NIH are developing and testing therapies for the virus; examining how other health conditions and our genes influence the disease’s severity; assessing the prevalence and transmissibility of the virus; and investigating the pandemic’s effects on mental health, fertility planning, and health disparities. Of course, covering all of these research efforts in a single blog would be impossible, and even describing a small subset ultimately proved too much for one post. As such, this blog — the first in a two-part series — will focus on several current IRP efforts to develop treatments for patients with COVID-19. Keep an eye out for another blog post in the coming weeks that will delve into still more examples of the many ways NIH researchers are studying the virus and its repercussions.
Launching a Direct Assault on the Novel Coronavirus
The wide range of expertise among IRP researchers has produced numerous projects that aim to treat COVID-19 from a variety of angles. For instance, IRP senior investigator Avindra Nath, M.D., is attempting to create DNA-like molecules called anti-sense oligonucleotides (ASOs) to treat the disease. These molecules bind to specific sequences found on the virus’s genome and trigger the infected cell to destroy them, thereby preventing the virus from replicating. Dr. Nath’s team has already designed several ASO molecules and is now beginning to test them in cells infected with the novel coronavirus.
Other IRP researchers hope to fast-track the drug development process by investigating whether existing medications for other ailments could prove effective against COVID-19. For example, researchers led by Wei Zheng, Ph.D., are screening a large set of FDA-approved medications and investigational drug candidates to see if any of them can stop the novel coronavirus from infecting cells, an effort that has already produced intriguing results. One segment of this project — a collaboration with scientists at Cornell University — is specifically focused on identifying compounds that prevent the coronavirus’s spike protein from binding to the ACE2 receptor on human cells, a necessary step for infection.
Antibodies like those pictured here help defend the body against viruses.
A third angle of attack against COVID-19 is searching the animal kingdom for special antibodies that can neutralize the virus. These antibodies, known as nanobodies, are smaller than human antibodies, allowing them to bind to sites on the novel coronavirus that larger antibodies cannot. Moreover, due to their small size and high stability, nanobodies could be given to patients via an inhaler, which makes them attractive potential therapeutics for respiratory infections like COVID-19. For these reasons, researchers led by IRP senior investigator Mitchell Ho, Ph.D., are searching for antibodies that can quash the novel coronavirus in a large library of nanobodies from camels and sharks that Dr. Ho’s lab had previously built. The team hopes that combining two or more nanobodies that can bind to different parts of the novel coronavirus might produce an effective antiviral therapy.
Revving Up the Immune Response
While many researchers are turning to lab-designed molecules or animals in their search for COVID-19 treatments, others are wondering whether simply giving our own immune system a boost could help patients fend off the virus. One of the the scientists pursuing this strategy is IRP senior investigator Thomas A Waldmann, M.D., whose studies focus on an immune molecule called interleukin-15, or IL-15 for short. IL-15 is released by certain immune cells in response to a viral infection and revs up the defensive response of other immune cells known as natural killer cells, which then begin destroying infected cells to limit the spread of the virus.
Dr. Waldmann’s group is investigating two different ways of using IL-15 to combat the novel coronavirus. The first involves incorporating it into COVID-19 vaccines in order to boost the immune response the vaccines stimulate. The second is to give IL-15 directly to patients either by itself or alongside antibodies that can bind to the virus in order to rev up natural killer cells’ assault on infected cells. The former approach could result in more effective vaccines to prevent infection in the first place, while the latter could help people who are already infected fight off the disease.
Curtailing the Consequences of COVID-19 Infection
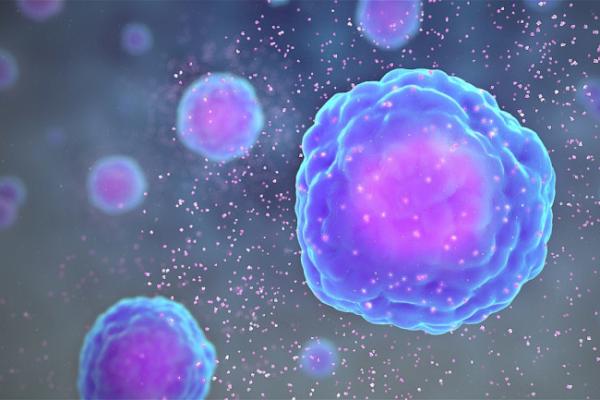
Some COVID-19 patients experience an immune system overreaction called a cytokine storm that results when immune cells release massive amounts of signaling molecules called cytokines. Image credit: scientificanimations.com/Wikimedia Commons.
While COVID-19 may be less lethal overall than many other infectious diseases, a significant portion of patients still experience severe and potentially life-threatening symptoms. As a result, a major focus of IRP coronavirus research is the development of strategies to lessen the virus’s effects on the body.
In some patients, the coronavirus triggers an immune system over-reaction known as a ‘cytokine storm,’ and multiple IRP projects are dedicated to finding ways to reign in patients’ rampaging immune cells. A team led by IRP senior investigator Robert Star, M.D., is testing strategies to mitigate cytokine storms in an animal model his lab had previously developed to study sepsis, an illness that occurs when an infection spurs a similar out-of-control immune response. Dr. Star’s group is examining the effects of a large number of FDA-approved and investigational drugs on the animals’ symptoms, as well as investigating whether treatments that target a pathogen-detecting protein called toll-like receptor seven (TLR7) might prevent or diminish a cytokine storm. The team is also looking into the possibility that a therapy utilizing capsules of chemicals called exosomes released by cells called mesenchymal stromal cells could curb the immune system’s overreaction to the novel coronavirus.

Dr. Edward Lakatta believes that treatments targeting the body’s renin-angiotensin system may curb COVID-19's ability to injure the lungs.
Meanwhile, an IRP team led by senior investigator Edward Lakatta, M.D., is pursuing the theory that interventions affecting the body’s renin-angiotensin system could help stop the virus from severely injuring patients’ lungs. This system controls numerous bodily functions, including regulating inflammation in the lungs, and it is influenced in part by the ACE2 protein that the novel coronavirus uses to infect cells. When the virus binds to ACE2 on the exterior of cells, the cells reduce how much ACE2 they produce, which limits ACE2’s ability to tamp down inflammation triggered by the renin-angiotensin system. Dr. Lakatta’s team plans to explore how age and sex affect ACE2 and the renin-angiotensin system, as well as whether interventions that change the functioning of the system affect the course of the disease in animal models of COVID-19 infection. The results of these studies could confirm the potential of targeting the renin-angiotensin system to reduce the damage COVID-19 does to the lungs.
The IRP has long played a vital role in fighting all manners of illness, and the COVID-19 pandemic is no exception. With hundreds of researchers at the NIH applying their expertise to defeating the novel coronavirus, important discoveries that will help save lives are surely on their way.
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs about the novel coronavirus and many other diseases from the NIH Intramural Research Program.
Related Blog Posts
This page was last updated on Tuesday, January 30, 2024
