
Robert A. Star, M.D.
Senior Investigator
Renal Diagnostics and Therapeutics Unit, Kidney Diseases Branch
NIDDK
Research Topics
The morbidity and mortality of acute kidney injury (AKI)—especially sepsis AKI—have remained high, despite numerous attempts at novel therapies. Many agents have worked in animals but failed in clinical trials. Effective treatment likely requires early detection and a better understanding of the pathophysiology of human AKI. Our long-term goals are to find markers to detect AKI and to develop therapies to treat and prevent AKI. We are developing better models that more closely mimic sepsis and sepsis AKI.
Clinically Relevant Sepsis Model of AKI
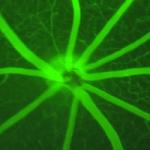
Sepsis is one of the leading causes of AKI, and 50 percent of patients with sepsis develop AKI. The pathogenesis of sepsis-induced AKI is very poorly understood. There are no drugs to treat sepsis-induced AKI, in part because of the lack of animal models that mimic the human disease. Therefore, we developed several new mouse models based on the cecal ligation and puncture model of polymicrobial sepsis, which has hyperdynamic and hypodynamic phases typical of human sepsis. To make the model realistic, we gave the animals pre-existing conditions (elderly animals or those with chronic kidney disease), and treated the animals with postoperative fluids and antibiotics. The mice developed biochemical and histological renal injury that was similar to human AKI. We are characterizing this model and using it to test treatment strategies. Because human sepsis is heterogeneous, a magic bullet approach will not work. Therefore, we are now developing companion precision selection biomarkers, and early drug response biomarkers that have allowed us to conduct a precision medicine clinical trial in mice with sepsis.
Biography
- M.D., Harvard Medical School-MIT, 1980
- B.A., Harvard University, 1976
Selected Publications
- Tsuji N, Tsuji T, Yamashita T, Hayase N, Hu X, Yuen PS, Star RA. BAM15 treats mouse sepsis and kidney injury, linking mortality, mitochondrial DNA, tubule damage, and neutrophils. J Clin Invest. 2023;133(7).
- Chung JY, Kim K, Ylaya K, Walker-Bawa KE, Perry C, Star RA, Hewitt SM. The Application of Guanidinium to Improve Biomolecule Quality in Fixed, Paraffin-embedded Tissue. J Histochem Cytochem. 2023;71(2):87-101.
- Andargie TE, Tsuji N, Seifuddin F, Jang MK, Yuen PS, Kong H, Tunc I, Singh K, Charya A, Wilkins K, Nathan S, Cox A, Pirooznia M, Star RA, Agbor-Enoh S. Cell-free DNA maps COVID-19 tissue injury and risk of death and can cause tissue injury. JCI Insight. 2021;6(7).
- Souza AC, Bocharov AV, Baranova IN, Vishnyakova TG, Huang YG, Wilkins KJ, Hu X, Street JM, Alvarez-Prats A, Mullick AE, Patterson AP, Remaley AT, Eggerman TL, Yuen PS, Star RA. Antagonism of scavenger receptor CD36 by 5A peptide prevents chronic kidney disease progression in mice independent of blood pressure regulation. Kidney Int. 2016;89(4):809-22.
- Street JM, Koritzinsky EH, Bellomo TR, Hu X, Yuen PST, Star RA. The role of adenosine 1a receptor signaling on GFR early after the induction of sepsis. Am J Physiol Renal Physiol. 2018;314(5):F788-F797.
Related Scientific Focus Areas


Molecular Biology and Biochemistry
View additional Principal Investigators in Molecular Biology and Biochemistry

This page was last updated on Thursday, August 7, 2025