IRP Researchers Tackle Coronavirus Crisis
New Studies Will Help Efforts to Contain and Treat COVID-19
Numerous recent IRP studies have yielded important information about the novel coronavirus currently spreading around the world.
Most of the time, science is a slow process, with many experiments taking years to yield results. However, as endeavors like the Manhattan Project have shown, scientists can dramatically accelerate the pace of discovery when necessary. Over the past few months, the novel coronavirus pandemic has spurred a burst of research from scientists around the world, including numerous IRP studies. Read on for a round-up of the latest IRP COVID-19 research and learn how IRP investigators are assisting in the fight against the novel coronavirus.
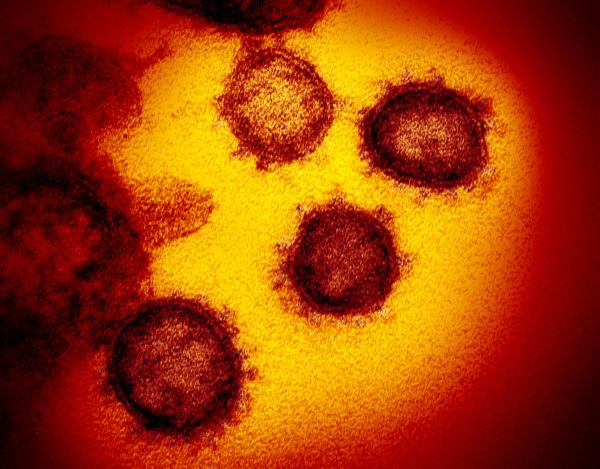
Scrutinizing Virus Survival Outside the Body
It is widely accepted that the main route by which COVID-19 is transmitted is inhaling virus-containing droplets of fluid released into the air when an infected person coughs or sneezes. However, it remains unclear how long the virus can survive in the open air or on surfaces that might transmit the disease when people touch them and then touch their faces. IRP researchers led by IRP senior investigator Vincent Munster, Ph.D., along with collaborators at institutions around the country, provided important insights into this question in a study published on March 17 as a Letter to the Editor in the New England Journal of Medicine.
The scientists found that particles of the novel coronavirus remained infectious for up to three hours in the air, up to four hours on copper surfaces, up to 24 hours on cardboard, and as long as three days on plastic and stainless steel. However, it is important to note that the amount of infectious virus in the air and on surfaces — and therefore the odds of contracting the virus through these routes — decreases dramatically as time passes. For example, the amount of infectious virus on plastic decreased by half after only seven hours. Moreover, not all of the viral particles on a surface will transfer to a hand that touches it. Finally, in order to become infected after touching an object, people must also touch their faces before washing or sanitizing their hands. Nevertheless, the study presents the possibility that the virus could spread through the air or contaminated objects.
Studying the Structure of the Coronavirus Spike
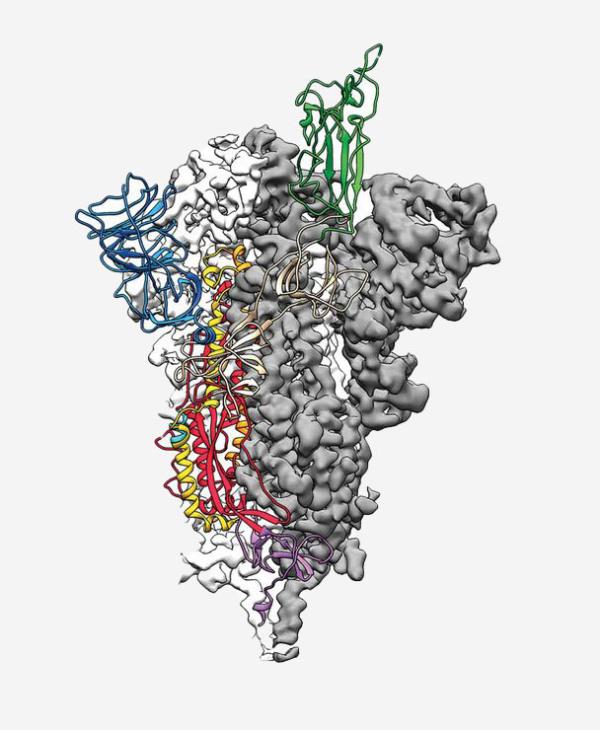
Side view of the novel coronavirus’ spike protein
The coronavirus that causes COVID-19 is one of several varieties of coronaviruses, all of which have proteins called spikes that stick out from their surfaces. These spikes interact with human cells to allow the viruses to infect them. In a study published on March 13 in Science, researchers in the lab of IRP senior investigator Barney Graham, Ph.D., and from the University of Texas at Austin used a technique called cryo-electron microscopy to visualize the structure of the novel coronavirus’ spike protein in three dimensions.
The researchers discovered that the virus’ spike binds to a receptor molecule on human cells more tightly than the spike of the closely related coronavirus that causes severe acute respiratory syndrome, or SARS. This finding could explain why the novel coronavirus behind the current pandemic is more infectious than the SARS virus, which infected more than 8,000 people in 26 countries during an outbreak in 2002 and 2003. In addition, knowing the atomic structure of the COVID-19 spike protein will accelerate efforts to develop a vaccine, as well as help scientists design therapeutic molecules that could help patients by binding to the spike protein and making it more difficult for the virus to infect cells.
Assessing an Animal Model of COVID-19 Infection
Humans aren’t the only animals that catch viruses like COVID-19. As a result, scientists can learn a great deal about infectious diseases by examining how they affect animals whose immune systems and other organs function similarly to our own. In a new study posted March 21 on the preprint server bioRxiv, a team of IRP scientists led by Emmie de Wit, Ph.D., studied how the novel coronavirus affects a species of primate called rhesus macaques. Preprints are preliminary reports that are shared prior to undergoing peer review in order to accelerate the dissemination of potentially useful information through the scientific community. Consequently, they should not be used to direct clinical practices until they have been peer reviewed.
Dr. de Wit’s team found that the monkeys’ symptoms were similar to those of human patients, including injury to the lungs. Scientists can now use this COVID-19 primate model to determine more precisely how the virus causes disease and to evaluate treatments and vaccines.
Testing Treatments to Protect the Lungs
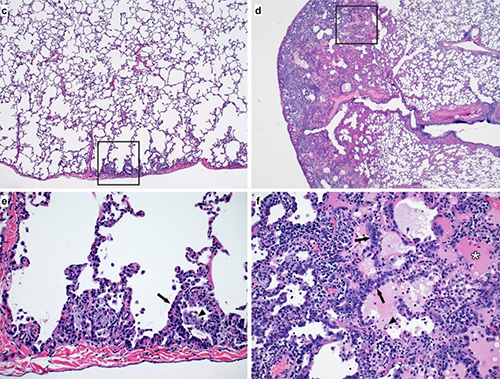
Examination of lung tissue from a primate model of COVID-19 infection (pictured here) revealed that the antiviral drug remdesivir helped protect the lungs from damage caused the virus.
In fact, less than a month after their preprint discussing the rhesus macaque model of COVID-19 infection appeared online, Dr. de Wit’s team posted another preprint on bioRxiv detailing a follow-up study in which they tested the antiviral medication remdesivir in that animal model. A six-day course of daily remdesivir treatment dramatically reduced the disease’s effect on the animals’ lungs. Moreover, even just 12 hours after their first treatment, the animals given remdesivir had much less virus in their lungs compared to animals given a placebo, though there was no difference in the amount of virus in the animals’ noses or throats. Lung samples from the animals examined a week after infection also contained much less of the virus in the animals given remdesivir compared to the placebo group. Finally, a week after infection, the lungs of the treated animals showed significantly less damage and fewer signs of pneumonia than the animals given the placebo.
The authors concluded that, if begun soon after infection, remdesivir treatment could help prevent severe lung damage in patients who have contracted COVID-19. However, because remdesivir failed to reduce the presence of the virus in the animals’ noses and throats, the researchers cautioned that patients given the medication may remain just as infectious despite improvement in their symptoms.
Shining a Light on Talking Transmission
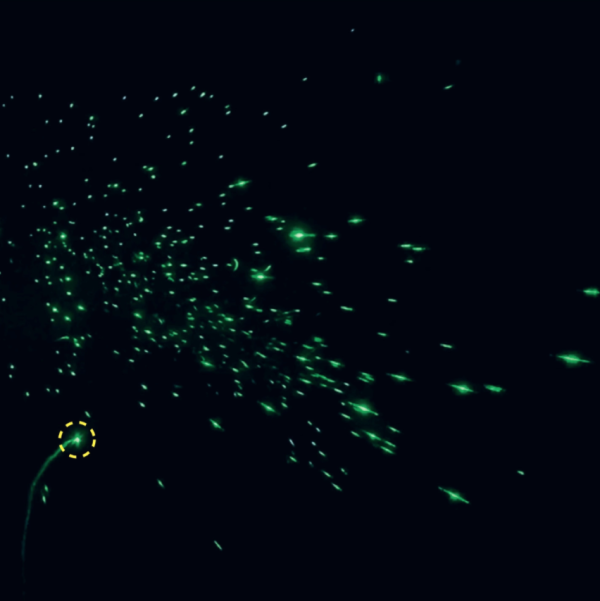
A green laser illuminates fluid droplets released from the mouth when speaking the phrase “stay healthy.”
Although COVID-19 primarily spreads via fluid droplets ejected from the body by a cough or sneeze, speaking also emits these droplets, raising the question of whether simply talking may transmit the virus from one person to another. To investigate this idea, a small group of scientists led by IRP senior investigators Philip Anfinrud, Ph.D., and Adriaan Bax, Ph.D., constructed a system that allowed them to see the droplets that were released by a person speaking. In their study, published on April 15 as a Letter to the Editor in the New England Journal of Medicine, a person spoke into a box painted black on the inside and a green laser lit up the droplets ejected from the speaker’s mouth.
While the study did not attempt to examine the likelihood of COVID-19 being transmitted via speech, the researchers did discover that saying the phrase “stay healthy” released a considerable number of fluid droplets from the mouth. Moreover, the louder the speech, the more droplets were produced. On the other hand, the same phrase produced no droplets when spoken through a slightly damp washcloth placed over the speaker’s mouth, providing further evidence for the value of face coverings in reducing the spread of the novel coronavirus.
Delving Into Decontamination of Critical Medical Equipment
Many recent news stories have discussed the shortage of critical personal protective equipment, or PPE, in the United States, without which medical personnel are much more vulnerable to becoming infected with COVID-19 while treating patients. Among the most important PPE are N95 respirator masks designed to protect the wearer from inhaling infectious particles. While these masks are designed to be used only once, IRP scientists and collaborators from the University of California, Los Angeles, have examined several potential methods of decontaminating the masks so they can be used multiple times. Their findings were recently written up in an April 15 preprint.

An N95 respirator mask
The researchers found that 60 minutes of exposure to dry heat above 70 degrees Celsius (158 degrees Farenheit) or exposure to ultraviolet light killed all the coronavirus particles on contaminated pieces of the fabric used to make N95 respirators. Decontamination with vaporized hydrogen peroxide, a commonly used antiseptic chemical, was also effective. However, three decontaminations via the ultraviolet light or heat treatment methods caused problems with the masks’ seal and fit over the face, suggesting that respirators decontaminated in these ways should only be reused twice. No such problems occurred when N95 respirator masks were treated with vaporized hydrogen peroxide, leading the authors to conclude that masks decontaminated with that chemical could be re-used three times. Knowing how to effectively decontaminate N95 respirators, as well as how many times decontaminated equipment can safely be reused, will help alleviate the PPE shortage and keep medical personnel healthy.
Counting Undetected Coronavirus Cases
A team of IRP scientists is currently recruiting volunteers for a new study that will shed light on how many American adults have antibodies for COVID-19 despite never having been officially diagnosed with the illness. Antibodies against the virus in a person’s blood indicate that individual was infected at one point, though he or she may not have been tested for COVID-19 or may have had no symptoms. By looking for antibodies in blood samples collected from as many as 10,000 participants, the study will provide crucial information about how widely the virus has spread in the United States and whether individuals from particular groups are more or less likely to contract the disease.
As these examples show, the NIH Intramural Research Program has leapt into the fight against COVID-19 with unprecedented speed and determination. The results of the IRP studies that have already been completed, as well as those that are now starting up or will be initiated in the near future, will increase our understanding of the disease and accelerate the creation of effective treatments and preventative measures.
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs about the novel coronavirus and many other diseases from the NIH Intramural Research Program.
Category: Science
Tags: COVID-19, coronavirus, vaccine, infectious disease, virus, cryo-EM, clinical
Related Blog Posts
This page was last updated on Tuesday, January 30, 2024
