Molecular Factors Underlie Mouth’s Head Start on Healing
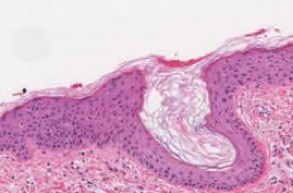
IRP researchers discovered the reason that skin tissue (pictured above) heals more slowly than tissue in the mouth.
As an impatient eater, I find myself burning or biting the inside of my mouth more often than I’d like. Fortunately, these injuries tend to heal within a day or two, whereas wounds like nicking my finger with a knife or scraping my knee seem to take a week or longer to disappear. My personal impressions have now been confirmed by a new NIH study that uncovered major differences in the way the mouth and skin repair themselves, pointing to potential therapeutic targets that could speed healing.1
While common injuries can take longer to mend than we’d like, certain conditions like the foot sores caused by diabetes heal agonizingly slowly or not at all. Such ‘chronic’ wounds can lead to infection or amputations and substantially reduce patients’ quality of life while driving up medical costs.
While clinicians have long believed that wounds to the inside of the mouth heal faster than skin injuries, these suspicions had never been scientifically validated. IRP investigators Maria Morasso, Ph.D., and J. Silvio Gutkind, Ph.D., set out to investigate those suspected disparities.
“Rather than rely on anecdotal evidence, we needed to learn whether it was a real difference,” says Dr. Gutkind, who has since moved to the University of California, San Diego. “Once we established it was real, we wanted to catalogue all the changes at the cellular and molecular levels that occurred in each place to explain why oral wounds heal faster than skin wounds.”
The researchers began by taking two tiny pieces of tissue from healthy volunteers — one from the skin under the armpit and one from the inside of the cheek — using a minimally painful biopsy technique routinely used by doctors. The scientists then examined the biopsy sites every three days for 15 days total. Some of the volunteers also had a second biopsy taken from the same locations either two or five days after the first.
The experiment confirmed that the oral biopsies healed much more quickly than the skin biopsies. In addition, by examining the activity of a wide array of genes in the two biopsy sites across the course of the study, the researchers discovered that numerous genes related to healing and infection prevention were already active in the mouth but not in the skin when the first biopsy was taken. Moreover, the activity of these genes rose in the skin in the days after the first biopsy but changed much less over time and quickly returned to the baseline level in the mouth tissue. The researchers concluded that the mouth is uniquely set up for healing, with important molecular processes already revved up and ready to go even before an injury occurs.
“The mouth is constantly having small abrasions due to chewing and it’s really rich in microorganisms, so you really want to make sure that the wound heals as quickly as possible,” Dr. Morasso says. “Those factors might have yielded pressures to develop mechanisms for quicker wound resolution compared to the skin.”
By comparing their own findings to those of related studies, the researchers were able to hone in on four specific genes that code for transcription factors, proteins that regulate the activity of other genes. Two of these transcription factor genes, PITX1 and SOX2, were much more active in cells from the uninjured mouth than cells from uninjured skin. Reducing the activity of PITX1 and SOX2 in mouth cells grown in petri dishes tamped down healing-related processes, whereas increasing their activity in skin cells ramped up those molecular pathways. Finally, mice genetically designed to have greater SOX2 activity in their skin healed much more quickly than mice with no SOX2 activity in their skin.
Dr. Morasso now plans to investigate the specific genes and molecular processes controlled by the transcription factors the study identified. Eventually, this research could help produce therapeutics that hasten healing and reduce scarring in both typical and chronic wounds. Dr. Gutkind, for his part, believes their work could provide insights into the development of oral cancers, which rely on the same cell division and movement processes that contribute to healing.
“Only in the NIH Intramural Research Program can these sorts of collaborations happen so quickly,” Dr. Gutkind says. “It’s a great example of team science where distinct but complementary expertise can be melded into something that is unique and would never have been able to be done individually.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Transcriptional signature primes human oral mucosa for rapid wound healing. Iglesias-Bartolome R, Uchiyama A, Molinolo AA, Abusleme L, Brooks SR, Callejas-Valera JL, Edwards D, Doci C, Asselin-Labat M, Onaitis MW, Moutsopoulos NM, Gutkind JS, Morasso MI. Sci Transl Med. 2018 Jul 25;10(451):eaap8798. doi: 10.1126/scitranslmed.aap8798.
Related Blog Posts
This page was last updated on Tuesday, January 30, 2024
