HIV Uses Host's Own Immune Molecules for Protection
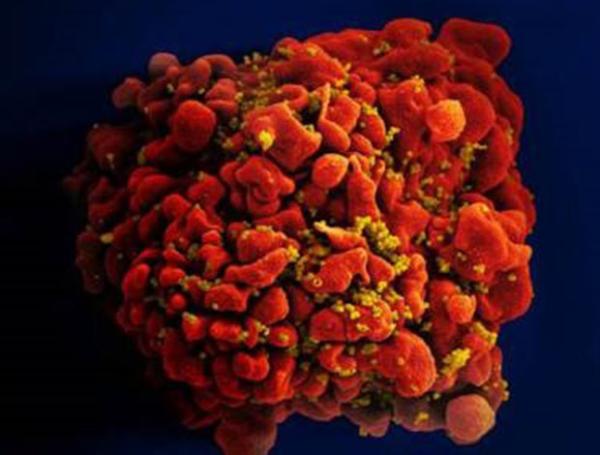
A team of IRP researchers has uncovered a promising avenue for helping the immune system eliminate HIV-infected cells like this one.
In one of Aesop’s classic fables, a clever wolf dons a sheep’s skin in order to move through the herd undetected. As it turns out, IRP researchers have discovered that in people with a specific set of immune system genes, the HIV virus uses a similar approach to hide from the body’s defenses.1
Nearly all cells in our bodies are coated with proteins called human leukocyte antigens (HLAs). These proteins allow the immune system to distinguish between healthy, native cells and those contaminated by unwelcome visitors like viruses or bacteria that must be destroyed. Each of the various HLA proteins is encoded by a different HLA gene and these genes vary considerably between individuals, causing different people to have different variants of each HLA protein.
“There are thousands of different forms of these HLA genes, and that variation allows us, as a species, to deal with virtually all infectious pathogens,” says IRP Senior Investigator Mary N. Carrington, Ph.D., the senior author of the new paper. “We’re really interested in the diversity of that part of the genome, since the risk of essentially every autoimmune disease, many cancers, and probably every infectious disease is associated with this set of genes.”
In their study, Dr. Carrington and her team first observed that HIV-positive individuals with a more active form of the HLA-A gene – resulting in more HLA-A protein on the surfaces of their cells – had more HIV virus in their blood, progressed faster to the severely weakened immune system associated with AIDS, and had fewer CD4+ T cells, the type of immune cell HIV infects and kills. In addition, in patients with a certain variant of the HLA-B gene, higher HLA-A gene activity led to even higher levels of the HIV virus.
The reason for those observations, the researchers found, was that those genetic variations inhibited natural killer cells, which provide the first line of defense against infection. A previous study had shown that the presence of that particular HLA-B gene variant increases the amount of a type of HLA, called HLA-E, on the surface of T cells2, and this new study showed that a more active HLA-A gene boosts HLA-E levels as well. HLA-E, in turn, inhibits natural killer cells by binding to a receptor on them called NKG2A, thereby preventing them from inadvertently attacking healthy T cells. The new research revealed that in HIV-positive individuals with high HLA-A gene activity and the problematic HLA-B variant, this method of reigning in natural killer cells impairs their ability to destroy T cells harboring the virus. As a result, like a wolf in sheep’s clothing, HIV is free to wreak havoc unchecked.
“People who have the ‘bad’ genotype – the genotype that enhances HLA-E expression – those people do poorly if they become infected with HIV,” Dr. Carrington says.
Fortunately, a drug that prevents HLA-E from binding to the NKG2A receptor is already being tested in clinical trials for rheumatoid arthritis and certain cancers, so Dr. Carrington hopes to repurpose that compound in an attempt to boost the body’s immune response against HIV. In a planned partnership with IRP Investigator Frank Maldarelli, Ph.D., she plans to test whether that strategy will encourage natural killer cells taken from HIV-positive patients to kill HIV-infected cells in a petri dish.
“The idea is to find out if this is a viable approach, in combination with other treatment regimens, to treat patients successfully,” Dr. Carrington explains. Unlike antiretroviral therapy, which often suppresses the HIV virus without completely eliminating it, she says, “the goal here is to cure the individual.”
Subscribe to our weekly newsletter to stay up-to-date on the latest developments in the NIH Intramural Research Program.
References:
[1] Elevated HLA-A expression impairs HIV control through inhibition of NKG2A-expressing cells. Ramsuran V, Naranbhai V, Horowitz A, Qi Y, Martin MP, Yuki Y, Gao X, Walker-Sperling V, Del Prete GQ, Schneider DK, Lifson JD, Fellay J, Deeks SG, Martin JN, Goedert JJ, Wolinsky SM, Michael NL, Kirk GD, Buchbinder S, Haas D, Ndung'u T, Goulder P, Parham P, Walker BD, Carlson JM, Carrington M. Science. 2018 Jan 5;359(6371):86-90. doi: 10.1126/science.aam8825. Epub 2018 Jan 4.
[2] Class I HLA haplotypes form two schools that educate NK cells in different ways. Horowitz A, Djaoud Z, Nemat-Gorgani N, Blokhuis J, Hilton HG, Béziat V, Malmberg KJ, Norman PJ, Guethlein LA, Parham P. Sci Immunol. 2016 Sep;1(3). Pii: eaag1672. Epub 2016 Sep 9.
Related Blog Posts
This page was last updated on Tuesday, January 30, 2024
