Immune Cells Produce Potent Packages of Anti-Inflammatory Molecule
Experimental Treatment Curbs Autoimmune Eye Disease in Mice
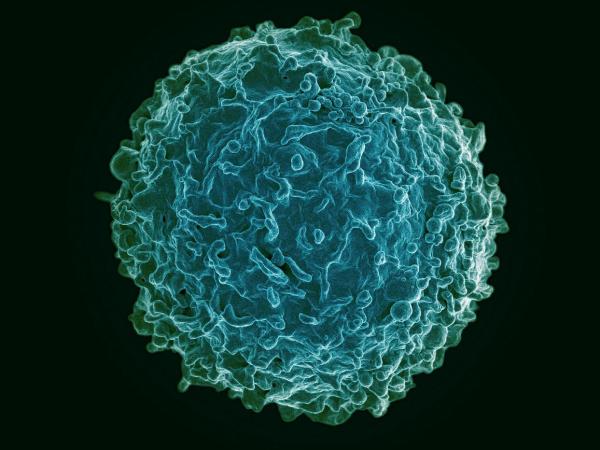
B cells like the one pictured here produce tiny packages of an anti-inflammatory molecule that could be used to treat autoimmune diseases, according to new IRP research.
Our cells produce a wide range of chemicals necessary for good health, but when they cannot manufacture enough of these substances, scientists can use cells cultivated in their labs to pick up the slack. In a promising example of this approach, IRP scientists stimulated lab-grown immune cells to produce tiny bundles of an important anti-inflammatory molecule and used those packages to successfully treat a potentially blinding autoimmune disease in mice.1
The light-sensing photoreceptor cells in the eye that allow us to see are extremely delicate and cannot regenerate. To protect them, a shield called the blood-ocular barrier walls off the eye from the rest of the body. However, in a group of eye diseases collectively known as autoimmune uveitis, out-of-control immune cells breach this barricade, ransack the eye, and destroy the photoreceptors. These conditions, which cause roughly 10 percent of visual handicaps in the United States, can cause irreversible blindness if left unchecked.
Doctors can treat autoimmune diseases with steroids and other medications that suppress the immune system, but putting shackles on a system that is meant to protect the body from invaders is not a viable long-term solution. To avoid the complications that can result from these treatments, scientists like IRP senior investigator Charles Egwuagu, Ph.D., have designed laboratory procedures for producing substances the body naturally uses to calm the immune system, including a chemical called interleukin 35, or IL-35 for short. Unfortunately, these efforts have been hindered by significant obstacles.
“IL-35 is difficult to manufacture,” says Dr. Egwuagu, the new study’s senior author. “We know it works, but to make it is very labor-intensive, and even if you have enough of it to use as a treatment, the body easily clears it.”
Another issue stems from the fact that IL-35 is made up of two subunits that must unite in order to exert an effect. Dr. Egwuagu’s lab has had success growing immune cells called B cells that naturally manufacture IL-35 and has seen promising results in studies using them to treat mouse models of autoimmune uveitis.2 However, because B cells secrete IL-35’s two parts separately, it is hard to predict how much active IL-35 they produce when introduced into a patient’s body.

Dr. Charles Egwuagu (left), the study’s senior author, and Dr. Minkyung Kang (right), the study’s first author.
His team’s new study presents a solution to this problem by showing that B cells grown in the lab also produce tiny packages called exosomes that contain both subunits of IL-35. When the IRP team repeatedly injected those exosomes into a mouse model of autoimmune uveitis over a period of several days, they found that the treatment curbed damage to the animals’ eyes and curtailed visual impairment. In addition, the exosome therapy reduced the abundance of a damaging, pro-inflammatory type of immune cell in the mouse’s eyes, spleens, and lymph nodes while increasing the number of ‘regulatory’ immune cells that inhibit their harmful counterparts in the animals’ eyes. And the effectiveness of the exosomes is not the only reason they might make for a desirable treatment.
“In these exosomes, the two subunits of IL-35 are together — they are sort of married,” Dr. Egwuagu explains. “As a result, you can predict and calculate how much active IL-35 is contained in a certain number of exosomes. We have to be able to know the dose we are using for a treatment, and with the exosomes, each time you use them, you know you’re getting the same dose.”
If future studies confirm the therapeutic effects of exosomes that contain IL-35, they could provide an easily scalable and safer alternative therapy for a variety of autoimmune diseases, including the neurological illness multiple sclerosis and graft-vs-host disease, a common complication of bone marrow and organ transplants in which immune cells in the donated tissue attack the recipient’s body. Dr. Egwuagu is now working on plans to test the exosome treatment in a mouse model of graft-vs-host disease. If the treatment works, the next step will be to try it out on people with autoimmune disorders.
“If you don’t show that a treatment works in humans, it doesn’t mean much,” Dr. Egwuagu says. “We’re not here to cure mouse diseases. This research is a prelude to an investigational new drug and pilot studies in human patients.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Interleukin 35-Producing Exosomes Suppress Neuroinflammation and Autoimmune Uveitis. Kang M, Choi JK, Jittayasothorn Y, Egwuagu CE. Front Immunol. 2020 May 29;11:1051. doi: 10.3389/fimmu.2020.01051.
[2] Interleukin-35 induces regulatory B cells that suppress autoimmune disease. Wang R, Yu C, Dambuza IM, Mahdi RM, Dolinska MB, Sergeev YV, Wingfield PT, Kim S, Egwuagu CE. Nat Med. 2014 Jun;20(6):633-41. doi: 10.1038/nm.3554.
Related Blog Posts
This page was last updated on Tuesday, January 30, 2024
