Taming Immune Cells with a Molecular “Switch”
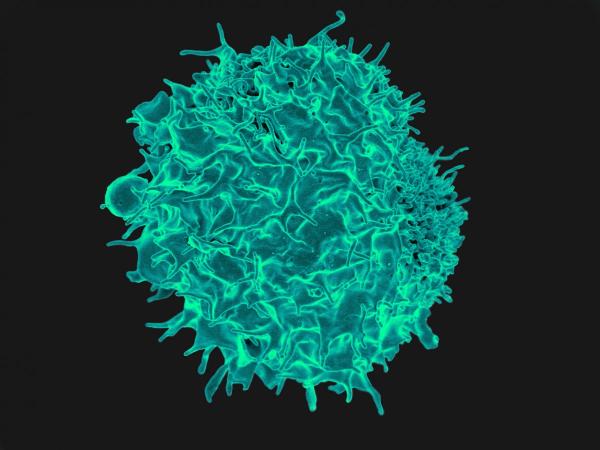
An IRP-led research team has discovered how a T-cell (pictured above) switches between secreting two chemicals that strengthen or weaken the body’s immune response.
The most important step to solving any problem is to choose the right tool for the job. Just like a heavy fur coat will keep you comfortable in the Arctic but slowly roast you in the Sahara, your immune system’s response can be helpful or harmful depending on the specific invader it’s fighting off. A new IRP study has identified a molecular “switch” that shifts an important type of immune cell between two different approaches to protecting the body.1
White blood cells called T cells play a critical role in the immune system. When they are not actively involved in intercellular combat, these cells remain in a default ‘naïve’ state, but once they sense a threat, they morph into a variety of subtypes that secrete different substances, called cytokines. Some cytokines are ‘inflammatory,’ meaning they ramp up the immune response, while others are ‘anti-inflammatory’ and have the opposite effect. For example, type 1 helper T cells (Th1 cells, for short) can release both the inflammatory cytokine interferon-gamma and the anti-inflammatory cytokine interleukin-10. If Th1 cells produce too much or too little of one of these chemicals, or secrete it at the wrong time, it can have dire consequences.2
“A certain kind of inflammation is necessary to fight off infection, so inflammatory cytokines are needed,” says IRP Senior Investigator Jinfang Zhu, Ph.D., the study’s senior author. “At the same time, the immune response needs to be dampened once the infection is controlled. So, it’s a balance — if you don’t control that response, then the T-cells’ activity becomes so overwhelming that the cytokines will kill the host.”
Th1 cells rely on molecules called transcription factors to carefully manage this balance. The key transcription factor for stimulating interferon-gamma production in Th1 cells is a molecule called T-bet. However, previous research by Zhu and his collaborators indicated that another transcription factor called Bhlhe40 is present at persistently high levels in Th1 cells,3 prompting them to investigate its specific role in the function of those cells.
To learn more about Bhlhe40, Zhu’s team developed a type of mouse whose T cells lacked the Bhlhe40 gene. While typical mice develop an inflammatory neurological condition called experimental autoimmune encephalomyelitis (EAE) when injected with a certain compound, the mice with no Bhlhe40 did not, suggesting that a lack of Bhlhe40 reduced inflammation. In another experiment, Zhu’s team gave T cells from either Bhlhe40-deficient mice or genetically normal mice to a type of mouse commonly used to study inflammatory bowel disease (IBD). These IBD-prone mice developed severe inflammation and lost weight when given normal T cells, but not when given T cells without Bhlhe40.
Further experiments revealed that Th1 cells without Bhlhe40 produced markedly less inflammatory interferon-gamma and much more anti-inflammatory interleukin-10, despite having typical levels of the T cell master regulator T-bet. Moreover, this imbalance had a profound effect on mice infected with Toxoplasma gondii, the parasite responsible for the disease known as toxoplasmosis. Whereas genetically normal mice survived the infection, the mice lacking Bhlhe40 all died within two to four weeks because they could not purge the parasites from their bodies. However, when the researchers partially blocked the action of interleukin-10 in the Bhlhe40-deficient mice, their bodies were able to fight off the pathogens and they survived.
“Interleukin-10 produced by Th1 cells is very important for regulating the immune response,” Dr. Zhu says. “Mice that don’t produce enough interferon-gamma cannot handle the infection, but mice lacking this negative regulator interleukin-10 will die because of an exaggerated inflammatory response, so the balance is very important.”
Dr. Zhu is now planning to examine whether the activity of the Bhlhe40 gene in individual Th1 cells is correlated with changes in the production of those two cytokines in genetically normal mice. Eventually, it may be possible to pharmacologically alter Bhlhe40 levels to either boost the body’s ability to combat infections or treat autoimmune diseases caused by an over-active immune system.
“A lot still needs to be done before we can apply this to disease,” Dr. Zhu says. “At this stage, we’re doing relatively basic studies, but I think we’re gaining answers to fundamental questions that are critical to the regulation of inflammatory and anti-inflammatory responses.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] The transcription factor Bhlhe40 is a switch of inflammatory versus anti-inflammatory Th1 cell fate determination. Yu F, Sharma S, Jankovic D, Gurram RK, Su P, Hu G, Li R, Rieder S, Zhao K, Sun B, Zhu J. J Exp Med. 2018 May 17. pii: jem.20170155. doi: 10.1084/jem.20170155.
[2] Conventional T-bet(+)Foxp3(-) Th1 cells are the major source of host-protective regulatory IL-10 during intracellular protozoan infection. Jankovic D, Kullberg MC, Feng CG, Goldszmid RS, Collazo CM, Wilson M, Wynn TA, Kamanaka M, Flavell RA, Sher A. J Exp Med. 2007 Feb 19;204(2):273-83.
[3] Expression and regulation of intergenic long noncoding RNAs during T cell development and differentiation. Hu G, Tang Q, Sharma S, Yu F, Escobar TM, Muljo SA, Zhu J, Zhao K. Nat Immunol. 2013 Nov;14(11):1190-8. doi: 10.1038/ni.2712.
Related Blog Posts
This page was last updated on Tuesday, January 30, 2024
