Rare Disease Research Reveals Why Immune Cells Go Wild
Discovery Could Improve Therapy for Multiple Autoimmune Diseases
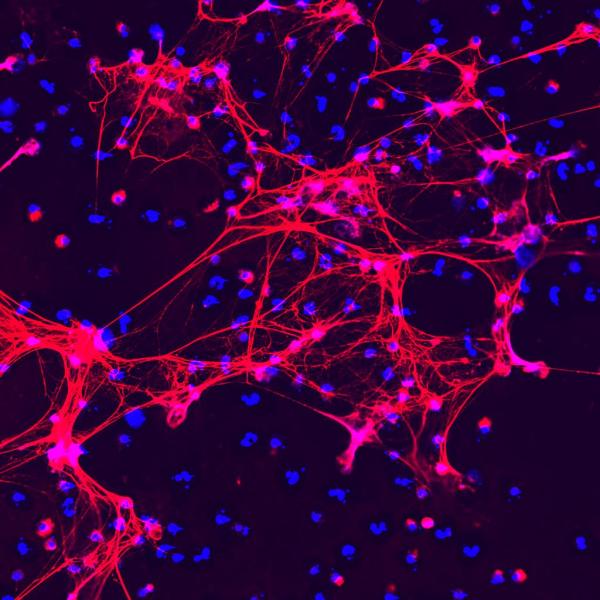
IRP researchers have discovered that toxic web-like structures called neutrophil extracellular traps (NETs), pictured above, cause the damage to blood vessels seen in an extremely rare autoimmune disorder.
Hiding among YouTube’s vast collection of cooking demos and funny cat videos are clips of patients and their advocates designed to raise awareness of specific diseases. It was just such a video that led IRP Senior Investigator Peter Grayson, M.D., M.Sc., to begin studying an extremely rare illness called deficiency of adenosine deaminase 2, or DADA2 for short. The recently published findings of that research could help improve treatment not just for patients with DADA2 but also many more individuals with similar ailments.1
Co-discovered in 2014 by IRP researchers led by Daniel Kastner, M.D., Ph.D.,2 DADA2 afflicts fewer than 200 known patients. The illness occurs when mutations disable both copies of a person’s ADA2 gene, which produces an enzyme called adenosine deaminase 2 (ADA2). DADA2 is a form of vasculitis, an ‘autoimmune’ condition in which the immune system attacks blood vessels, leaving them damaged and inflamed. In the most severe cases, the condition can cause strokes and bleeds in the brain.
Dr. Grayson began studying DADA2 after seeing a video on YouTube about a mother and her two children with another form of vasculitis called polyarteritis nodosa (PAN). This situation struck Dr. Grayson as odd because PAN does not run in families. DADA2, on the other hand, does.
“I had just learned about the work from Dan Kastner’s team on DADA2 and I was pretty sure that woman and her children had DADA2,” Dr. Grayson recalls, “so we brought them into the Clinical Center and genetically tested them and they had the disease.”
Dr. Grayson’s team — which included staff scientist Carmelo Carmona-Rivera, Ph.D., the paper’s first author, and Mariana Kaplan, M.D., Chief of the IRP's Systemic Autoimmunity Branch — soon began examining blood and tissue samples from patients with DADA2. The scientists found that when the patients’ symptoms were at their worst, their blood contained many more immune cells called neutrophils, which are the earliest responders to infections and injuries. In addition, a sample of inflamed tissue from a patient with DADA2 contained large numbers of neutrophil extracellular traps (NETs), toxic chemical webs that neutrophils use to kill bacteria but that can also damage tissue and cause inflammation.
What’s more, patients with DADA2 had much higher levels of a chemical called adenosine in their blood than healthy individuals. Because the ADA2 enzyme that individuals with DADA2 lack breaks down adenosine, the researchers wondered if the patients’ excessive levels of adenosine were causing their neutrophils to over-produce NETs. Subsequent experiments showed that the more adenosine that neutrophils were exposed to, the more NETs they produced, but this effect was blunted when ADA2 was added to the mix.
Surprisingly, the IRP researchers also found that female patients’ neutrophils produced more NETs when exposed to adenosine than those from male patients. This could help explain why autoimmune diseases are much more common in women than men.
“In a lot of those diseases neutrophils also play a big role,” Dr. Grayson says, “so maybe this is the tip of the iceberg to help us start to understand the role that sex may play in some of these diseases.”
Adenosine affects the behavior of immune cells by binding to four different receptors on the cells’ exteriors. The IRP team found that adenosine spurred less NET formation by neutrophils when the cells were also exposed to chemicals that blocked a specific type of adenosine receptor called A1. A synthetic chemical that activates the A1 adenosine receptor, on the other hand, triggered neutrophils to produce more NETs.
An examination of immune cells called macrophages further supported the idea that excessive NET production in patients with DADA2 contributes to the rampant inflammation in their bodies. Exposing macrophages to NETs produced by patients’ neutrophils caused the macrophages to secrete much larger amounts of an inflammatory molecule compared to when the macrophages encountered NETs created by healthy individuals’ neutrophils. However, activating the A2 adenosine receptor on the macrophages stopped NETs from stimulating macrophages’ production of inflammatory molecules.
The IRP research points towards the potential to treat individuals with DADA2 by altering the way immune cells respond to adenosine, which would be a much more targeted, disease-specific approach than current treatments. Therapies that target the adenosine system might also be a boon to patients with similar autoimmune ailments like PAN, lupus, and rheumatoid arthritis.
“These rare diseases don’t exist in a vacuum,” Dr. Grayson says. “I think this study really highlights the value of rare disease research because you learn things that likely have broader implications for a wider range of patients and conditions.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Deficiency of adenosine deaminase 2 triggers adenosine-mediated NETosis and TNF production in patients with DADA2. Carmona-Rivera C, Khaznadar SS, Shwin KW, Irizarry-Caro JA, O'Neil LJ, Liu Y, Jacobson KA, Ombrello AK, Stone DL, Tsai WL, Kastner DL, Aksentijevich I, Kaplan MJ, Grayson PC. Blood. 2019 Jul 25;134(4):395-406. doi: 10.1182/blood.2018892752.
[2] Early-onset stroke and vasculopathy associated with mutations in ADA2. Zhou Q, Yang D, Ombrello AK, Zavialov AV, Toro C, Zavialov AV, Stone DL, Chae JJ, Rosenzweig SD, Bishop K, Barron KS, Kuehn HS, Hoffmann P, Negro A, Tsai WL, Cowen EW, Pei W, Milner JD, Silvin C, Heller T, Chin DT, Patronas NJ, Barber JS, Lee CC, Wood GM, Ling A, Kelly SJ, Kleiner DE, Mullikin JC, Ganson NJ, Kong HH, Hambleton S, Candotti F, Quezado MM, Calvo KR, Alao H, Barham BK, Jones A, Meschia JF, Worrall BB, Kasner SE, Rich SS, Goldbach-Mansky R, Abinun M, Chalom E, Gotte AC, Punaro M, Pascual V, Verbsky JW, Torgerson TR, Singer NG, Gershon TR, Ozen S, Karadag O, Fleisher TA, Remmers EF, Burgess SM, Moir SL, Gadina M, Sood R, Hershfield MS, Boehm M, Kastner DL, Aksentijevich I. N Engl J Med. 2014 Mar 6;370(10):911-20. doi: 10.1056/NEJMoa1307361.
Related Blog Posts
This page was last updated on Wednesday, May 24, 2023
