Brain Pathway Amplifies Pain After Injury
Mouse Study Could Aid Development of Treatments for Chronic Pain

IRP research has demonstrated that the connection between two brain areas plays a key role in how the body experiences pain after an injury.
Getting hurt or sick is bad enough, but millions of patients around the world continue to experience pain or hypersensitivity even after their ailment resolves itself. Despite the prevalence of chronic pain, few effective treatments are available, especially ones without the potential for addiction that opioid medications carry. However, new IRP research has shown that suppressing the electrical firing of neurons in a certain brain area can alleviate injury-induced hypersensitivity in mice, providing a promising new target for treatments aimed at relieving chronic pain.1
Pain is both physical and psychological — after all, it is just a sensation like any other, and the brain must add an emotional component to it to make it unpleasant. That combination of features has led pain researchers like IRP investigator Yarimar Carrasquillo, Ph.D., the new study’s senior author, to focus on a part of the brain called the amygdala, which not only receives information about physical sensations, but also plays an important role in processing emotional information.
“I fell in love with the amygdala because I felt like it integrates both of these components of pain,” Dr. Carrasquillo says. “When you think about pain, especially chronic pain in particular, the issue is not just the ‘ouch’ component. It’s also quality of life. When you talk to patients, they will say that it bothers them that they cannot work anymore — there’s a lot of missed work. They’re grumpy. It affects their social life. They’re depressed, sad, anxious, and all of those emotional aspects are known to be mediated by the amygdala.”
One of Dr. Carrasquillo’s most important discoveries about the amygdala is that two different populations of neurons in the central amygdala dial up and tamp down pain, respectively, similar to how tuning a thermostat adjusts a building’s temperature. Meanwhile, other scientists have shown that one of the main brain areas that relays pain-related information from the spinal cord to the central amygdala is the parabrachial nucleus (PBN), so in her lab’s recently published study, her team explored the role that connections between the PBN and central amygdala might play in chronic pain.

Top: Yarimar Carrasquillo, the study’s senior author. Bottom: Jeitzel Torres-Rodriguez (right) and Torri Wilson (left), the study’s co-first authors
“This pathway is going to tell you that you are in pain or you’re experiencing an injury,” explains former IRP postbaccalaureate IRTA fellow Jeitzel Torres-Rodriguez, the study’s co-first author along with IRP biologist Torri Wilson. “It’s the first filter that tells your body to react to the injury or not.”
Indeed, when the IRP researchers pinched the paws of mice, neurons in the PBN became more active, including those that send signals to the central amygdala. However, when the scientists examined the behavior of PBN neurons that connect to the central amygdala in mouse models of a nerve injury, they found that the injury did not change how much the cells fired even though the affected paw subsequently became much more sensitive to cold, heat, pressure, and prodding with a small, blunt metal rod. This unexpected result suggests an injury may not alter the electrical activity within the PBN, but rather turn up the volume of the signals it sends out when they are received by the central amygdala.
Not satisfied with merely observing the behavior of the neural connection between the PBN and central amygdala, Dr. Carrasquillo’s team next used a genetic manipulation to give themselves the ability to directly control the electrical signals the PBN sends to the central amygdala. In mouse models of nerve injury, suppressing those signals in this way eliminated the affected paw’s hypersensitivity to temperature and other types of stimulation, so much so that the animals' responses were the same as when the researchers prodded or applied heat or cold to one of their paws that was not affected by the nerve injury. On the other hand, increasing the PBN’s electrical signaling to the amygdala caused hypersensitivity to cold, pressure, and poking sensations — but not to heat — in healthy mice.
“When we activate this pathway in animals that don’t have an injury, they behave as if they were injured,” Dr. Carrasquillo says.
Finally, the researchers examined what would happen if they curbed the PBN’s electrical communication with the central amygdala after injecting an inflammation-inducing chemical into a paw of otherwise healthy mice. This animal model more closely resembles the ‘spontaneous’ pain not linked to any clear source that is often experienced by patients with chronic pain. The IRP team found that suppressing PBN activity had the same effects as in the nerve injury model, once again reducing hypersensitivity to all the different types of sensations the scientists applied to the affected paw.
“If you look at patients, they’re not complaining because someone is poking them,” Dr. Carrasquillo points out. “Often, they’re feeling pain even though nothing is happening, so this model is used in our field to look at spontaneous pain responses.”
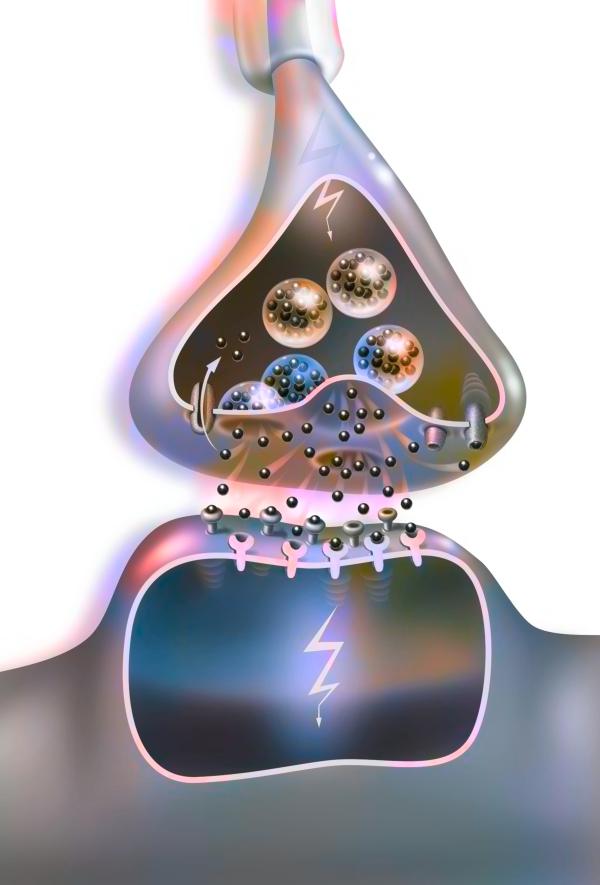
Electrical signals from neurons cause the release of chemicals called ‘neurotransmitters.’ Dr. Carrasquillo hopes identifying the specific neurotransmitters released in the central amygdala when PBN neurons fire could lead to better treatments for chronic pain.
Taken together, the study’s results provide strong evidence that communication between the PBN and central amygdala may play an important role in some types of chronic pain. Dr. Carrasquillo’s lab is now conducting similar experiments looking at how manipulating that neural pathway influences animals’ behavior over longer periods of time, as well as investigating the specific chemicals that are released in the central amygdala when the PBN is activated. Identifying those specific ‘neurotransmitters’ could lead to effective treatments for chronic pain that have fewer side effects than treatments that target chemicals used all around the brain for many different purposes.
“We cannot target more common neurotransmitters like glutamate or GABA because those are everywhere, so we’re trying to identify neurochemicals that are released in injured states but that are kind of dormant in uninjured states, so that way treatments will be more selective,” Dr. Carrasquillo says.
“We now have multiple papers that show you can drive pain-like behaviors in otherwise completely healthy animals, and I think that gives hope to so many patients who have pain and are frustrated because they keep going to the doctor and they have no other apparent health problems, and their doctors are telling them they can’t find anything,” Dr. Carrasquillo adds. “It might be because we’re looking at the wrong place. We need to pay more attention to the brain and identify how to treat pain as a neurological problem.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Torres-Rodriguez JM, Wilson TD, Singh S, Torruella-Suárez ML, Chaudhry S, Adke AP, Becker JJ, Neugebauer B, Lin JL, Martinez Gonzalez S, Soler-Cedeño O, Carrasquillo Y. The parabrachial to central amygdala pathway is critical to injury-induced pain sensitization in mice. Neuropsychopharmacology. 2023 Aug 4. doi: 10.1038/s41386-023-01673-6.
Related Blog Posts
This page was last updated on Wednesday, January 31, 2024
