Treating Parkinson’s Disease with Pinpoint Precision
Drug Candidate Could Slow Progression and Reduce Side Effects

IRP researchers are developing a drug that, when taken alongside other treatments, could more effectively slow the progression of Parkinson’s disease while reducing side effects.
If you know someone with Parkinson’s disease, you’re probably familiar with the progressive tremors and movement difficulties it causes. Unfortunately, the most common treatment for the disease — a drug called levodopa, or L-DOPA for short — can make some movement problems worse when taken for long periods of time. That’s why IRP senior investigator David R. Sibley, Ph.D., and postdoctoral fellow Amy Moritz, Ph.D., have taken on the challenge of discovering new drugs that could be given to patients in conjunction with existing treatments to more effectively slow the disease’s progression while reducing side effects.
At the root of Parkinson’s disease lies a chemical called dopamine, a ‘neurotransmitter’ that sends messages between nerve cells, or neurons. It affects many life-sustaining physiological processes, including heart rate and kidney function, as well as pain, movement, learning, mood, and attention. Consequently, physical and psychological problems can ensue when dopamine levels are altered or there are problems with the molecular ‘receptors’ that dopamine interacts with to exert its effects.
In the brains of people with Parkinson’s disease, dopamine-producing neurons degenerate and stop sending signals in the brain. As dopamine levels drop, people develop physical symptoms such as tremors, stiffness, and poor balance and coordination. To complicate matters, there are actually five different dopamine receptors that vary slightly in structure and function. L-DOPA and similar drugs cannot differentiate between these receptors and end up interacting with the wrong ones or all of them at once.
“That’s a problem if you’re trying to develop drugs to target individual receptor subtypes,” explains Dr. Sibley. “A lot of drugs available today cross-react with other receptors and that can lead to side effects.”
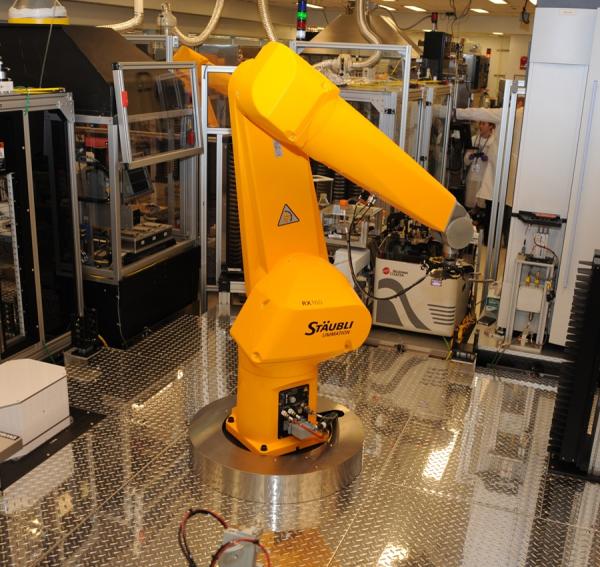
High-throughput screening uses robots like this one to test huge numbers of drug candidates for their effects on a particular molecule, cell type, or harmful organism.
Although the search for more effective drugs to treat Parkinson’s has gone on for years with limited success, it wasn’t until the NIH opened the National Center for Advancing Translational Sciences (NCATS) in 2011 that Dr. Sibley turned his attention from basic biology research to drug discovery. NCATS provides IRP scientists the ability to perform high-throughput drug screening, enabling researchers to search through hundreds of thousands of chemical compounds for ones that could be useful as medications. The robotic process, which was inspired by the automated equipment used on automobile assembly lines, uses large plastic or glass plates with thousands of tiny spaces where large numbers of candidate drug compounds can be mixed with specific targets, such as pathogens like bacteria or cells that have receptors for molecules like dopamine, to see if there is some sort of beneficial interaction. In this way, scientists can test large numbers of compounds in one go, or many slightly different versions of a single compound. The latter capability comes in handy when trying to refine a drug with a known effect.
“You go through many rounds of testing slightly different versions of a starting compound to see what changes on the molecule improve activity and selectivity and which changes decrease activity,” Dr. Moritz explains.
Drs. Moritz and Sibley, in collaboration with IRP staff scientist Benjamin Free, Ph.D., began their quest for a more targeted Parkinson’s treatment by creating a molecular test that looked for interactions between candidate molecules and a particular dopamine receptor, known as the D3 receptor. The test was designed such that a successful interaction between a potential drug and the D3 receptor produced a tiny but measurable amount of light with the help of a fluorescent molecule. With this tool in hand, the IRP duo and their colleagues at NCATS were able to use NCATS’ high-throughput screening robots to sift through all of the nearly 400,000 compounds in NCATS’ small molecule library to find something that worked. In fact, they actually conducted the screen twice: once looking for ‘antagonists’ that shut down the D3 receptor and once to find ‘agonists’ that activate the receptor.

Dr. Amy Moritz
Eventually, they winnowed down NCATS’ collection of potentially useful compounds until they found one that was highly selective for the D3 receptor, meaning it interacted strongly with that receptor and weakly or not at all with other types of dopamine receptors. Next, the IRP team worked with Kevin Frankowski, Ph.D., a medicinal chemist at the University of North Carolina, to enhance the compound’s effects on the D3 receptor by synthesizing and testing versions of it with slightly different structural modifications. At the end of the process, they ended up with a promising drug candidate called ML417.1
“In our manuscript, we showed that ML417 is actually the most selective D3 agonist currently known,” Dr. Sibley says. “We then worked with a computational chemist at NIH, Dr. Lei Shi, to learn why this compound is so selective. We found that it interacts with the D3 receptor in a way that is unique compared with other molecules that activate that receptor.”
In addition, Drs. Sibley and Moritz, in collaboration with IRP clinical fellow Emmanuel Akano, M.D., tested ML417’s ability to protect against a toxin that kills off neurons that release dopamine. The IRP scientists found that ML417 protected isolated dopamine-producing nerve cells from the toxin’s effects.
Dr. David Sibley
“When people are diagnosed with Parkinson’s disease, up to 80 percent of their dopamine neurons have already died,” Dr. Sibley says, “so if you have a protective compound, you can try to save the remaining 20 percent. That would be helpful in slowing the disease’s progression.”
Due to ML417’s specific effects on D3 receptors, it has great potential as a medication to curb movement problems associated with Parkinson’s disease. Since these problems can also be a side effect of Parkinson’s treatments, the IRP team hopes to use ML417 as the basis for a drug that can be taken in conjunction with L-DOPA and other treatments to stave off this aspect of the disorder. While further work is needed, recent preliminary experiments in animal models, conducted in collaboration with IRP senior investigator Judith Walters, Ph.D., suggest that ML417 can provide such therapeutic effects. Meanwhile, Dr. Moritz and Dr. Sibley have also continued testing related molecules for their effects on D3 receptors in search of one that inhibits the receptor as selectively and potently as ML417 activates it.
“We did find some D3-selective antagonists in the high-throughput screen, so we chose the best one and are basically doing the same medicinal chemistry as we did with ML417 to create a highly selective drug,” says Dr. Moritz.
Alongside its efforts to combat Parkinson’s disease, the IRP team is partnering with colleagues outside NIH to test the idea that inhibiting D3 receptors may be useful for preventing relapse in people who are dependent on opioid painkillers and are trying to stop using them. That sort of ‘translational’ work — transforming their knowledge of how dopamine receptors work into actual treatments for patients — is an exciting next step for Dr. Sibley and Dr. Moritz.
“Translational science is just so important,” notes Dr. Sibley. “It’s the way forward for developing novel therapeutics for treating many different diseases and disorders.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Moritz AE, Free RB, Weiner WS, Akano EO, Gandhi D, Abramyan A, Keck TM, Ferrer M, Hu X, Southall N, Steiner J, Aubé J, Shi L, Frankowski KJ, Sibley DR. Discovery, optimization, and characterization of ML417: A novel and highly selective D3 dopamine receptor agonist. J. Med. Chem. 2020; 63(10):5526-5567. doi.org/10.1021/acs.jmedchem.0c00424.
Related Blog Posts
This page was last updated on Wednesday, May 24, 2023
