An Unlikely Target in the Fight Against Alzheimer’s
IRP Researchers Find Link Between Dementia and Byproducts of Cholesterol Breakdown

Molecules called bile acids created when the body breaks down cholesterol could be involved in Alzheimer’s disease and other forms of dementia, according to recent IRP research.
When most people think about Alzheimer’s disease, the liver is probably the organ least likely to come to mind. Yet recent IRP research suggests that molecules called bile acids, which are synthesized in the liver, may influence the development of Alzheimer’s disease.1 In honor of Brain Awareness Week this week, we’re diving into that work to learn how such an unlikely target could help lead to new treatments for Alzheimer’s and other forms of dementia.
To date, efforts to develop therapies for Alzheimer’s disease, which affects more than 6 million Americans over the age of 65, have achieved little success. Many scientists are focused on proteins in the brain as potential treatment targets, including the ‘amyloid-beta’ protein now infamous amongst Alzheimer’s researchers. In contrast, IRP senior investigator Madhav Thambisetty, M.D., Ph.D., has been exploring the role that cholesterol might play in the development of Alzheimer’s and vascular dementia, which is marked by microscopic bleeding and blood vessel blockage and is the second most common form of dementia.
“We’ve known for many years that high levels of blood cholesterol are associated with dementia, but we really don’t fully understand how this works,” he explains. “Since high cholesterol is recognized as a metabolic abnormality, it was sort of a natural question to ask and get to the bottom of this mystery.”
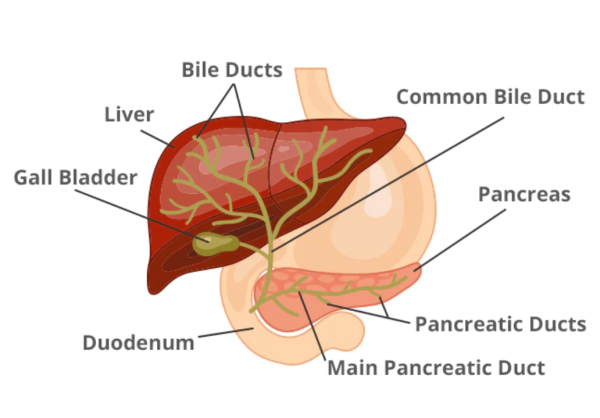
When the liver breaks down cholesterol, the resulting bile acids are stored in the gallbladder, which can then release them into the body to participate in various biological processes.
Cholesterol in the blood cannot cross the blood–brain barrier, but molecules called bile acids that are produced when the liver breaks down cholesterol can. Consequently, Dr. Thambisetty and his team theorized that bile acids might explain the connection between high blood cholesterol levels and Alzheimer’s risk. To investigate their theory, they conducted three analyses using data from a variety of sources, including patient medical records, brain scans, brain tissue, and blood samples collected repeatedly from the same individuals over long periods of time.
In their first analysis, which examined brain scans and medical data collected by an IRP-led initiative called the Baltimore Longitudinal Study of Aging (BLSA), Dr. Thambisetty’s team found a relationship between lower bile acid levels in the blood and higher amounts of amyloid-beta plaques in the brain, which have long been associated with Alzheimer’s disease. Low amounts of bile acids in participant’s blood were also associated with faster atrophy of brain tissue.
“That was one of the first significant discoveries in this study,” says Dr. Thambisetty. “And what’s interesting is that this appears to be different in males and females.”
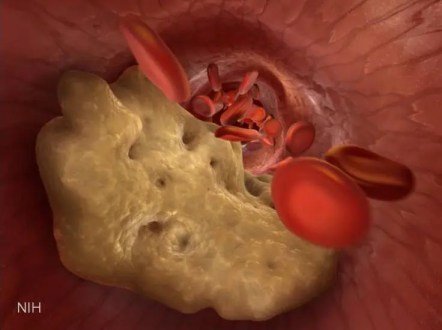
When cholesterol lodges in the walls of blood vessels, it can form plaques that disrupt blood flow, cause inflammation, and raise the risk for heart attacks and strokes. As a result, many people take cholesterol-lowering medications like statins.
To better understand this relationship and find a possible explanation for the sex differences, his team next compared the risk for dementia in individuals who were prescribed an older class of cholesterol-lowering drugs called bile acid sequestrants and those taking other drugs to bring down their cholesterol levels. Bile acid sequestrants were the first line of defense before the now more commonly used statin drugs were introduced, and they are still used for patients who can’t tolerate the newer medications. They work by binding to bile acids in the blood and ensuring that they are removed from the body. The body senses the shrinking supply of bile acids and breaks down more cholesterol to restore their levels, resulting in lower blood cholesterol.
Although the overall risk for dementia was similar in the two sets of patients, when Dr. Thambisetty’s team separated the data by sex, men taking bile acid sequestrants had a higher risk of developing vascular dementia than men taking other types of drugs. The researchers also found that dementia risk increased the longer a man had been taking bile acid sequestrants.
“This observation complements our earlier finding that lowering these bile acids in the blood is associated with measures of brain atrophy and amyloid accumulation,” notes Dr. Thambisetty.

More From the IRP
Blog Post
Dietary Supplement Powers Alzheimer’s-Afflicted Neurons
Finally, his team used tissue samples collected from deceased individuals to try to identify a precise mechanism behind those observations. This led to the discovery that, compared to healthy people, patients with dementia have altered activity in genes related to sites in the brain that bile acids bind to, known as bile acid receptors. Specifically, those genes were either over-active or under-active in individuals with signs of dementia. This finding adds further weight to the idea that systems in the brain that are influenced by bile acids may be a promising target for dementia treatments.
“This work feeds into a much larger motivation for my group, which is to try and understand mechanisms associated with Alzheimer's disease, but to do so in a way that brings us closer to effective treatments,” Dr. Thambisetty says. “That is the big motivation for all of our work.”

Dr. Madhav Thambisetty
Dr. Thambisetty’s team is now examining whether experimental compounds that affect bile acid receptors can reduce abnormalities associated with Alzheimer’s disease in cell and animal models of the illness. The group is also sifting through data on large numbers of patients for evidence that Alzheimer’s risk can be diminished by commonly used medications prescribed for other illnesses that work by targeting those receptors.
“If there is a drug that's widely used in hundreds of thousands of individuals, then we can go to these large real-world clinical data sets and compare people who have been exposed to the drug to people who have not in order to determine whether the drug lowers risk for Alzheimer's disease,” he explains.
By using drugs that have already made it through many stages of evaluation, such as testing for safety and efficacy, and even approval by the U.S. Food and Drug Administration (FDA), scientists can overcome some of the initial hurdles of getting a drug to patients.
“I think a lot of the work that we do as researchers, at least for me personally, is informed by this underlying motivation,” Dr. Thambisetty says. “The questions that we've chosen to focus on here, if answered, will be of tangible benefit to my patients.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Bile acid synthesis, modulation and dementia: a metabolomic, transcriptomic and pharmacoepidemiologic study. Varma Vr, Wang Y, An Y, Varma S, Bilgel M, Doshi J, Legido-Quigley C, Delgado JC, Oommen AM, Roberts JA, Wong DF, Davatzikos C, Resnick SM, Troncoso JC, Pletnikova O, O’Brien R, Hak E, Baak BN, Pfeiffer R, Baloni P, Mohmoudiandehkordi S, Nho K, Kaddurah-Daouk R, Bennett DA, Gadalla SM, Thamisetty M. PLoS Med. 2021 May 27;18(5):e1003615. doi: 10.1371/journal.pmed.1003615.
Related Blog Posts
This page was last updated on Wednesday, May 24, 2023
