Neuron-Killing Protein Exploits a Vulnerability in Mitochondrial Armor
Study Shows How Molecular Trespasser Gains Entry into Cells’ Energy Producers
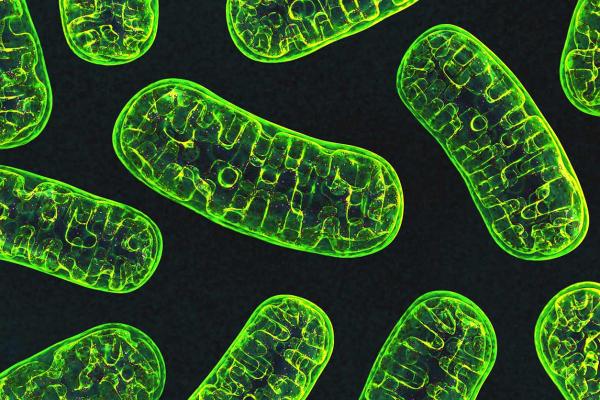
Our cells’ energy-producing mitochondria (pictured above) have tight security to make sure harmful substances cannot interfere with their crucial function. New IRP research has discovered how a toxic protein linked to neurodegenerative diseases bypasses these defenses to damage mitochondria in neurons.
As a fan of the long-running animated sitcom The Simpsons, I’ve witnessed the bumbling Homer Simpson cause several near-meltdowns at the nuclear power plant where he works. Serious problems can arise at such facilities when the wrong person gains access to them, and the same applies to the energy-producing mitochondria that power our cells. A new IRP study has revealed how a protein known to harm neurons gains entry into mitochondria in order to wreak cell-killing havoc.1
Parkinson’s disease, a debilitating neurological condition that causes severe movement problems, is the second-most common neurodegenerative disorder in the U.S. The disease is associated with abnormal accumulation of a protein called alpha-synuclein that is naturally produced in neurons. Past studies have shown that when alpha-synuclein builds up in cells, it somehow moves inside mitochondria and interferes with their ability to produce the energy cells need to survive. However, the access point alpha-synuclein uses to enter mitochondria has long been a mystery.
A clue to this puzzle emerged several years ago when a French pharmaceutical company discovered that a drug called olesoxime protects mitochondria from the toxic effects of excess alpha-synuclein.2 The company’s scientists also found that olesoxime binds to a protein found on the outer surface of mitochondria called the voltage-dependent anion channel, or VDAC3, which acts as a gateway to permit certain molecules to move into and out of mitochondria.
Those observations intrigued Tatiana Rostovtseva, Ph.D., an associate scientist in the lab of IRP senior investigator Sergey Bezrukov, D.Sc., Ph.D., because her lab’s studies have shown that alpha-synuclein also interacts with VDAC.4 Consequently, Dr. Rostovtseva and a postdoctoral fellow in her lab, Amandine Rovini, Ph.D., set out to determine if VDAC is involved in olesoxime’s ability to protect mitochondria from alpha-synuclein.
“Think of VDAC as a large pore in the mitochondria’s outer membrane,” explains Dr. Rostovtseva. “It’s like a checkpoint. Most of the substances that mitochondria process or produce could not cross the outer membrane without VDAC.”
Dr. Rostovtseva (second from the left), Dr. Rovini (fourth from the right), and their colleagues in Dr. Bezrukov’s lab
Working with members of their own lab and Parkinson’s disease researchers in the lab of IRP senior investigator Mark Cookson, Ph.D., Dr. Rostovtseva and Dr. Rovini ultimately proved their hunch was correct. The team began by inducing an over-production of alpha-synuclein in a type of cell that is commonly used to study neuronal function. Consistent with past studies, they found that excess alpha-synuclein killed those cells and that olesoxime treatment dramatically reduced the rate of cell death by keeping mitochondria healthy. The IRP team also confirmed that when the cells over-produced alpha-synuclein, much more alpha-synuclein was found inside their mitochondria and in close proximity to VDAC on the outer surface of the mitochondria. However, olesoxime treatment significantly decreased the amount of alpha-synuclein located close to VDAC, as well as the amount of the protein inside the mitochondria.
Next, to examine whether VDAC was necessary for alpha-synuclein to gain entry into mitochondria, the scientists dramatically reduced the amount of VDAC in cells that over-produced alpha-synuclein. Without VDAC, they discovered, alpha-synuclein could not accumulate inside mitochondria, proving for the first time in a cell model that VDAC is the gateway through which alpha-synuclein enters mitochondria. Moreover, additional studies provided evidence that olesoxime protects mitochondria from alpha-synuclein by hindering alpha-synuclein’s ability to pass through VDAC.
“This is a very new mechanism we’re proposing,” says Dr. Rostovtseva. “I think this explains a lot of things, and it is also probably not unique to alpha-synuclein or olesoxime. VDAC is a main mitochondrial site affected in many neurodegenerative diseases, and olesoxime is just one of a number of neuroprotective and anti-cancer drugs that interact with VDAC, so this mechanism could be applicable to drugs other than olesoxime as well.”
For example, it may be that cancer drugs often cause a form of nerve damage called neuropathy because, like alpha-synuclein, they harm mitochondria by passing through VDAC. If this is found to be the case, studies like Dr. Rostovtseva’s could point towards potential methods of reducing this side effect. Her team’s discoveries could also have important implications for the treatment of numerous neurological diseases that, like Parkinson's, result from the death of neurons, including ALS and Huntington’s disease.
“Whether we use olesoxime or not to treat these diseases, studies like ours show us where to focus,” says Dr. Rostovtseva. “VDAC has not been of much interest because it’s just a hole, but from my point of view, VDAC and other proteins in the mitochondria’s outer membrane have been overlooked. If our hypothesis is right, it means that we need to focus the research community on considering VDAC as a pharmacological target for drugs.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Molecular mechanism of olesoxime-mediated neuroprotection through targeting α-synuclein interaction with mitochondrial VDAC. Rovini A, Gurnev PA, Beilina A, Queralt-Martín M, Rosencrans W, Cookson MR, Bezrukov SM, Rostovtseva TK. Cell Mol Life Sci. 2019 Nov 23. doi: 10.1007/s00018-019-03386-w.
[2] Protective role of olesoxime against wild-type α-synuclein-induced toxicity in human neuronally differentiated SHSY-5Y cells. Gouarné C, Tracz J, Paoli MG, Deluca V, Seimandi M, Tardif G, Xilouri M, Stefanis L, Bordet T, Pruss RM. Br J Pharmacol. 2015 Jan;172(1):235-45. doi: 10.1111/bph.12939.
[3] Olesoxime (TRO19622): A Novel Mitochondrial-Targeted Neuroprotective Compound. Bordet T, Berna P, Abitbol J, Pruss RM. Pharmaceuticals (Basel). 2010 Feb; 3(2): 345-368. doi: 10.3390/ph3020345
[4] α-Synuclein Shows High Affinity Interaction with Voltage-dependent Anion Channel, Suggesting Mechanisms of Mitochondrial Regulation and Toxicity in Parkinson Disease. Rostovtseva TK, Gurnev PA, Protchenko O, Hoogerheide DP, Yap TL, Philpott CC, Lee JC, Bezrukov SM. J Biol Chem. 2015 Jul 24;290(30):18467-77. doi: 10.1074/jbc.M115.641746.
Related Blog Posts
This page was last updated on Tuesday, January 30, 2024
