Bugs, the Brain, and Behavior
The Gut Microbiome’s Role in Addiction
We’ve all had that gut feeling, a prescient awareness telling us that something is amiss—or conversely that something is perfectly right indeed. But could our gut also influence us in other ways, such as how we engage in addictive behaviors? The concept of this bidirectional communication system, called the gut-brain axis, has been well established. Hardwiring our brainstem to our intestines is the vagus nerve. Hormones and other molecules produced in the gastrointestinal tract broker communication between the brain and gut via neuroendocrine pathways.

CREDIT: NHGRI
The microbial communities that live in and on our bodies play a role in health and disease. NIH scientists have recently found that an imbalance in the healthy versus unhealthy microbes in our gut may play a role in neuropsychiatric conditions such as alcohol-use disorder (AUD) and other addictive behaviors.
Then there’s the bugs. Our microbiome—teeming communities of diverse microbes that live on and within us—plays an integral role in human physiology from the proper functioning of the immune system to the digestive system. Acting through the gut-brain axis, an imbalance in healthy versus unhealthy gut flora, a condition known as dysbiosis, has been linked to disorders such as anxiety, depression, and obesity. Now researchers are asking a different question: Could dysbiosis be a part of the puzzle in neuropsychiatric conditions such as alcohol-use disorder (AUD) and other addictive behaviors? Recent research suggests it might.
Binge drinking is one risk factor for developing AUD. For men that means consuming five or more alcoholic drinks on an occasion (in about two hours); for women, it’s four or more. Binge drinking represents a massive public health problem in the United States and is associated with automobile injuries, gun violence, and domestic violence, and can lead to serious diseases. Of great concern is that the earlier an individual starts binge drinking, the higher the risk of developing AUD.
There are only three approved medications and a small number of effective behavioral interventions to treat AUD, and so it is critical to shed light on how it develops and to find new diagnostic tools and therapeutic targets.

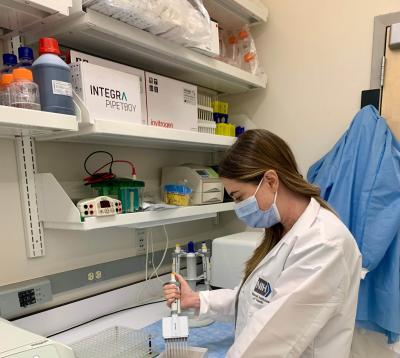
CREDIT: NIDA
Lorenzo Leggio’s lab is studying the gut microbiome and neuroendocrine pathways to better understand mechanisms underlying addiction and to develop new treatments.
Identifying addiction pathways
Seeking to understand mechanisms underlying addiction and to develop new treatments is physician-scientist and Senior Investigator Lorenzo Leggio, who heads the Clinical Psychoneuroendocrinology and Neuropsychopharmacology (CPN) Section, a joint National Institute on Drug Abuse and National Institute on Alcohol Abuse and Alcoholism (NIAAA) translational and clinical laboratory. CPN conducted pioneering work demonstrating in rat models and humans that ghrelin, commonly known as the hunger hormone, influences addictive behaviors such as alcohol craving and excessive consumption. Moreover, they found that when rats were given alcohol at a binge level for many weeks their gut microbiome tipped into the dysbiotic, leading to a decrease in microbial diversity compared with controls (J Neuroendocrinol DOI:10.1111/jne.12663, 2018).
Might those findings be relevant to people? Leggio’s group next collaborated with Elise Weerts at Johns Hopkins Bayview Medical Center (Baltimore) and Claire Fraser at the University of Maryland Institute for Genome Sciences (Baltimore). Weerts established a baboon model of binge drinking that has been proven to be effective at screening for new medications that could potentially be used in clinical trials. Using this model, the research team studied how the baboon’s microbiome and metabolome—consisting of bioproducts such as proteins and peptides generated from cells—changed in response to chronic alcohol drinking.
Three groups of male olive baboons (Papio anubis) were studied: The control group drank Tang to match the calories consumed by the alcohol-binge-drinking groups. A second group had been binge drinking for approximately two years and the third had been drinking heavily for about 10 years. Surprisingly, a marked difference was discovered only in the microbiome and metabolome of the 10-year drinking group. Populations of beneficial gut bacteria in the Lachnospiraceae and Prevotellaceae families declined, whereas the opportunistic pathogen in the Streptococcus genus increased. The long-term-drinking baboons also showed an increase in markers of oxidative stress and certain microbe metabolites that were not present in the control or two-year drinking groups (Transl Psychiatry 11:609, 2021).
Leggio found the results intriguing. “Our findings tentatively suggest that alcohol doesn’t just change the microbiome and metabolome in a transient way,” he said. “You need chronic, prolonged, binge drinking in order to lead to a sustained change.”
A causal link between the microbiome and brain has yet to been shown, but it’s important to demonstrate that alcohol alters the microbiome because accurate biomarkers to make neuropsychiatric diagnoses are lacking. If microbial changes are a consequence of chronic binge drinking, then those changes could be a way to objectively identify people with unhealthy alcohol use.
Currently, the CPN lab is analyzing data from a recent NIAAA outpatient clinical trial conducted at the NIH Clinical Center (CC) that compared healthy control subjects to individuals with AUD. That study promises to test associations between alcohol use in humans and changes in the microbiome and metabolome, as well as how those factors interact to influence behavior and physiology.
Future research at CPN looks to investigate whether an unhealthy gut could precede the development of AUD or play a role in maintaining it. “If that were true,” said Leggio, “then you could pharmacologically manipulate the gut microbiome as a way to treat AUD.” He pointed to preliminary evidence in a human study from Belgium showing that dysbiosis in the gut correlated with increased alcohol craving (Proc Natl Acad Sci USA 111:E4485-E4493, 2014). Craving is a critical predictor of recurrence in substance-use disorders.

CREDIT: NIAAA
Lorenzo Leggio’s lab is analyzing data from a completed outpatient clinical study that included a craving (cue-reactivity) procedure in a bar built in a laboratory. Laboratory-based bars have been used to study medication effects, cue reactivity, and alcohol-use expectancies in social and dependent drinkers. Pictured: Lorenzo Leggio.
Experimental treatments
So what might new therapeutic approaches look like for AUD? Using a procedure called fecal microbiota transplant (FMT), a small NIH-funded study at Virginia Commonwealth University (VCU) in Richmond, Virginia, transplanted stool into 20 volunteers with severe AUD and liver cirrhosis. Half of the participants received a placebo implant and the other half received bacteria from a healthy person’s stool. Compared with the control group, FMT recipients showed an increase in beneficial gut bacteria and had higher concentrations of short-chain fatty acids (SCFAs)—an important microbial byproduct that helps maintain intestinal lining integrity. Excessive intestinal permeability is thought to leak toxins into the body and has been associated with several inflammatory and mental health conditions and AUD. Nine of the participants treated with FMT experienced a short-term reduction in craving and drank less, compared with only three in the placebo group (Hepatol DOI:10.1002/hep.31496, 2020).
In a follow-up study, the VCU team demonstrated that the behavioral changes observed after FMT could be transmitted through microbial transfer: Mice colonized with post-fecal-transplant stool (from the human participants of the first study) reduced their acceptance of, intake of, and preference for alcohol compared with pre-fecal-transplant colonized mice and control mice who received a sterile transplant (Nat Comm 13:6198, 2022).
Leggio noted the vast diversity of human microbiota varies depending on factors such as age, sex, race, and co-morbidities. Thus, manipulating the gut microbiome, even if proved effective in future large studies, might not work out for every patient. Other researchers have proposed a related treatment option of increasing dietary fiber intake, which has been linked with better mental health by boosting SCFA production.
NIH-funded scientists are also exploring how FMT might be used to treat alcohol-related liver disease (ALD), in which the microbiome may play a role in the effects of alcohol on the liver. In parallel with rising unhealthy alcohol use in the United States and worldwide, ALD rates have also been increasing, with the largest surge seen in young people and women. Without effective interventions for AUD, the mortality rate for ALD is expected to double by 2040.
Searching for a brain-bug connection
The benefits of abstaining from alcohol or reducing the consumption of it are well known and may extend to our gut health, too. Researchers in the Clinical Center’s Translational Biobehavioral and Health Disparities Branch (TBHD)—including Bioinformatics Scientist Jennifer Barb and Principal Investigator and Chief Gwenyth Wallen—collaborated with NIAAA scientists in a clinical study with 22 newly abstinent inpatients with AUD. The group found that the patients’ gut microbiomes began to recover over the course of four weeks, becoming more diverse and healthier (Gut Microbes 11:1608–1631, 2020).

CREDIT: MELODY YAZDANI
Jennifer Barb (pictured) and Chief Gwenyth Wallen in the Clinical Center’s Translational Biobehavioral and Health Disparities Branch collaborated on a clinical study with scientists in the National Institute on Alcohol Abuse and Alcoholism. They found that the gut microbiomes became more diverse and healthier in people with alcohol-use disorder who had recently abstained from drinking alcohol.
Since that study, improved genomic-sequencing technology has associated specific genera of gut microbes, such as Morganella, with mental-health disorders such as depression and anxiety, which are common in patients with AUD. TBHD Assistant Clinical Investigator Katherine Maki and Barb are collaborating with Reza Momenan (Director of NIAAA’s Clinical Neuroimaging Research Core) on a retrospective secondary analysis of the data from the abstinence trial. They are incorporating comprehensive genomic sequencing of the gut microbiome samples with structural-magnetic-resonance-imaging scans to determine whether activity in certain regions of the brain related to stress might correlate with the presence of suspected pathological microbes and with symptoms such as sleep disturbance, anxiety, depression, alcohol withdrawal, and craving.
CREDIT: JENNIFER BARB, CC
Katherine Maki, in the Clinical Center’s Translational Biobehavioral and Health Disparities Branch, is part of a team that is analyzing functional-MRI data from patients with alcohol-use disorder to determine if activity in certain brain regions correlate with changes in the gut microbiome.
A holistic approach
People with substance-use disorders often present with several medical issues that may also be linked to addictive behavior. In many cases, people with AUD have severe oral-health problems, such as periodontitis, and are sent for a dental workup by National Institute of Dental and Craniofacial Research (NIDCR) clinicians when they come into the CC (Open Forum Infect Dis 6:S895–S896, 2019). To better treat the whole person, TBHD is designing a new protocol with an interdisciplinary team of investigators from NIDCR and NIAAA to study the oral microbiome, oral-health status, and general oral-health practices in those patients.
Barb noted that this holistic approach is a missing component in research, and important to understand given the mouth’s close proximity to the brain. For example, bacteria in the mouth from a highly infected tooth could have implications on the brain through byproducts produced in the bloodstream.
“There could be a bidirectional relationship with oral health, the brain, AUD, and poor oral hygiene because you are under the influence [of alcohol],” she said.
Opposite of the gut, less microbial diversity in the mouth is thought to be healthier. Previously, TBHD found that the oral microbiome in patients who abstained from alcohol did indeed become healthier and assessments of oral health improved during the course of inpatient treatment. Furthermore, oral microbial changes were associated with the type of alcohol that the patient consumed, with overall diversity being lowest among wine drinkers (J Oral Microbiol 14:2004790, 2022).
TBHD scientists are not only treating the immediate causes of AUD, but also educating those patients on the importance of sleep and proper nutrition, both of which have “a major influence on the gut microbiome,” said Barb. “We want to think about the whole person and help patients to not only stop drinking, but [also] think about all the components of health when they leave.”
The study of our bugs’ role in behavior is still in its infancy. And what we uncover may turn out to be a more universal picture of the pathways that integrate our resident microbial activity with our own physiology.
“From an evolutionary standpoint the body cares less about distribution, organizational charts, and chain-of-command,” said Leggio. “It’s a democratic system. All organs, components, and residents in our body are important and have a voice!"
To learn more
Other NIH scientists are studying the microbiome, too, including Distinguished Investigator Yasmine Belkaid at the National Institute of Allergy and Infectious Disease, and Senior Investigator Julie Segre at the National Human Genome Research Institute, who spearheaded NIH’s Human Microbiome Project. Researchers such as Leggio and Senior Investigator Andrew Holmes (NIAAA) have also collaborated with renowned gut-brain axis expert John Cryan at University College Cork (Cork, Ireland). To watch Cryan’s lecture at NIH on the gut-brain-axis go to [https://videocast.nih.gov/watch=17162]. And to hear a lecture by Claire Fraser about the microbiome and genomics hosted by former NIH Director Francis Collins, go to [https://videocast.nih.gov/watch=40165].

Michael Tabasko is the Science Writer-Editor for The NIH Catalyst.
This page was last updated on Thursday, March 16, 2023
