Robot-Assisted Experiments Point to Treatments for Rare Cancer
Study Identifies Drugs That Exploit the Disease’s Weak Spots

With the help of some robots like those pictured here, IRP researchers have discovered promising new ways to treat a rare form of skin cancer.
The best way to destroy a cancer cell is to target its weak points, but that’s obviously easier said than done, especially when you want to kill those diseased cells while sparing healthy ones. That’s where robots come in, allowing scientists to quickly evaluate the effects of thousands of drugs on cancer to see what works and what doesn’t. IRP researchers recently used that approach to identify potential treatments for a rare skin cancer, including a strategy that appears to be particularly good at hitting the disease where it’s most vulnerable.1
When skin cancer comes to mind, most people think of the most common forms, like melanoma and basal cell carcinoma. This means rare varieties, like Merkel cell carcinoma, receive little public attention or research funding. However, that variety of cancer has long been on the mind of IRP senior investigator Isaac Brownell, M.D., Ph.D., the new study’s senior author, who is seeking to expand the treatment options for it beyond the immunotherapies that are the current first-line treatment.
“They actually work great for Merkel cell carcinoma — in fact, it’s one of the solid tumors that responds best to immunotherapy — but despite that, more than 50 percent of the patients who are treated don’t have a durable response, so we do need an alternative treatment for more than half of these patients,” he says.
To that end, Dr. Brownell’s lab recently teamed up with several other IRP research groups to use robots for quickly testing nearly 4,000 different drugs for their effects on Merkel cell carcinoma, about 2,400 of which have already been approved to treat other diseases by the U.S. Food and Drug Administration or similar entities in other countries. What’s more, the researchers examined the drugs’ effects on both varieties of Merkel cell carcinoma: virus-positive, which is caused by the cancer-causing virus Merkel cell polyomavirus, and virus-negative, which is caused by mutations in certain skin cells due to environmental exposures like ultraviolet light. The drug screen also included non-cancerous cells so the researchers could distinguish between drugs that kill Merkel cell carcinoma specifically and drugs that are toxic to all cells, including the ones we want to keep around.
The drug screen showed that 39 of the drugs tested killed the cancer cells without harming the normal cells at all: 14 that affected both virus-positive and virus-negative Merkel cell carcinoma, 23 that only affected the virus-positive cells, and 2 that only affected virus-negative cells. In addition, when the researchers relaxed their criteria slightly by sifting through the data for drugs that reduced the survival of all cells, but had a much greater effect on the cancer cells, they ended up with 131 candidates: 18 that affected both varieties of the cancer, 98 that only affected the virus-positive cells, and 15 that only affected virus-negative cells.

Dr. Isaac Brownell
“There’s an old joke that you can kill cancer in a dish with lots of things, including battery acid, but you wouldn’t want to pour battery acid into your cancer patients,” Dr. Brownell says. “We need to find those things that kill cancer better than they kill other cell types.”
The next step the IRP scientists took was to group the promising drugs identified by the screen based on the specific biological processes they are known to interfere with. This analysis yielded an interesting finding: several of those drugs are known to inhibit a family of enzymes called aurora kinases, which cells need to divide properly. That discovery was supported when the researchers performed another automated experiment that individually reduced the activity of more than 10,000 different genes in Merkel cell carcinoma cells. The experiment showed that knocking down the activity of the gene for aurora kinase B noticeably reduced the survival of both virus-positive and virus-negative cancer cells, though it was more effective in killing the former type.
“Aurora kinase inhibitors are effective in a lot of types of cancer, but as you can imagine, drugs that affect dividing cells affect many types of cells that are dividing in our body, such as those in the bone marrow and the gut, and that’s part of their limitations,” Dr. Brownell explains. “The thing about Merkel cell carcinoma is it’s so sensitive to these aurora kinase inhibitors that we can use them at lower levels to avoid the toxicity we see to other tissues. It’s so great at killing Merkel cell carcinoma that we’re hopeful we’ll be able to find a way to use them in the clinic without causing too many side effects.”
As expected based on the team’s findings so far, when they looked at the effects of an aurora kinase B inhibitor called AZD2811, which is currently being tested in clinical trials for other cancers, the drug interfered with the division of both types of Merkel cell carcinoma, causing them to die. And once again, it had more of an effect in virus-positive than virus-negative cells. What’s more, giving the drug to mice with either virus-positive or virus-negative Merkel cell carcinoma tumors engrafted into their skin yielded extremely promising results.
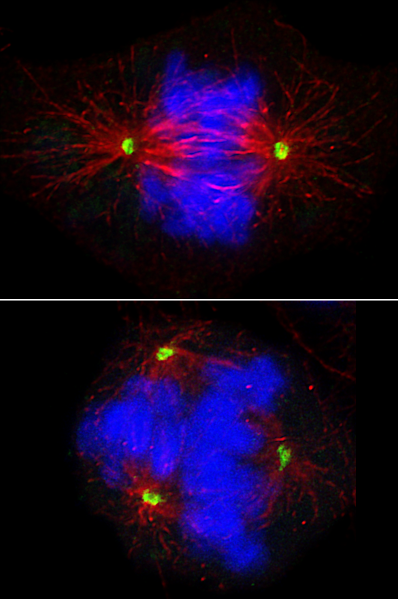
Top image: A Merkel cell carcinoma cell dividing to make two daughter cells. Bottom: Disrupted cell division in a Merkel cell carcinoma cell caused by treatment with an aurora kinase B inhibitor. The cells’ chromosomes appear in blue, while the mitotic spindle, which is needed to divide up the chromosomes evenly between daughter cells, is shown in red. Images by Drs. Khalid Garman and Davide Randazzo
“We test drugs in these pre-clinical mouse models all the time, and most people consider it a success if you can slow the growth of the tumor by half,” Dr. Brownell says. “With AZD2811, we shrank existing tumors, and in the case of the virus-positive tumors, even when we stopped treating the mice, their tumors didn’t grow back. That is extremely uncommon — like a jaw-dropping positive result.”
Given those impressive outcomes, Dr. Brownell believes there is great potential for aurora kinase B inhibitors as a treatment for patients with Merkel cell carcinoma who are not cured by immunotherapy. However, that was just one approach that his team’s study identified, and his lab plans to continue investigating the effects of many of the drugs that proved effective against Merkel cell carcinoma, both as singular treatments and in combination.
“One of the beautiful things about the screen we did is that we looked at drugs that were already FDA-approved,” he says. “We found drugs that inhibit aurora kinase B had a lot of potential, but we also saw a lot of other drugs that we’re following up on, including some drugs approved for other diseases that we could repurpose for our patients with Merkel cell carcinoma. When you’re treating a rare disease, that’s often the fastest way to get a new drug to patients.”
“Industry doesn’t like to invest in things that have limited potential for economic returns, and people who are at other research institutions often choose to study diseases that are more common,” he adds. “That leaves this dearth of people who are investigating rare diseases like Merkel cell carcinoma, so I think it’s important that NIH does that type of work and supports scientists like myself and my collaborators to tackle these rare diseases. And when we discover things in these rare diseases, it doesn’t just help the patients who have rare cancers, but we make discoveries about how to combine therapies and attack cancer as a more general entity, and sometimes we make discoveries that have implications beyond our immediate patient population. You never know where discovery is going to happen when it comes to biomedical research.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Gelb T, Garman KA, Urban D, Coxon A, Gryder B, Hill NT, Miao L, Lee T, Lee O, Chakka S, Braisted J, Jarvis JE, Glavin R, Raj TS, Xiao Y, Difilippantonio S, Wang AQ, Shen M, Cheng KC, Lal-Nag M, Hall MD, Brownell I. High-throughput screening identifies Aurora kinase B as a critical therapeutic target for Merkel cell carcinoma. Nat Commun. 2025 Feb 12;16(1):1583. doi: 10.1038/s41467-025-56504-7.
Related Blog Posts
This page was last updated on Tuesday, April 29, 2025
