Leveraging AI To Combat Cervical Cancer
IRP Researcher Identifies Precise Disease Biomarkers

IRP research has produced a prototype algorithm that could one day help doctors more quickly and accurately detect cervical cancer in its early stages.
Over the last few decades, advances in cervical cancer screening and prevention have fundamentally changed the approach to dealing with one of the most common forms of cancer in younger women. While doctors have been able to detect cancerous and pre-cancerous cells with a Pap smear since the 1940s, the more recent discovery that the human papillomavirus (HPV) causes more than 90 percent of cervical cancers now affords greater accuracy to regular screening tests. What’s more, IRP researchers truly changed the game by developing a vaccine against HPV, which was approved by the U.S. Food and Drug Administration (FDA) in 2006.
Still, despite these extremely positive developments, much work remains to be done, as cervical cancer continues to kill about 4,000 American women each year. In honor of World Cervical Cancer Awareness Month this January, we spoke with IRP Senior Investigator Nicolas Wentzensen, M.D., Ph.D., about his efforts to bring that number as close to zero as possible.
“The HPV vaccine works best when it’s administered before onset of sexual activity,” says Dr. Wentzensen, and not everyone eligible receives it at that point in their lives. “And then there’s a large population out there that is not protected by the vaccine, who still strongly benefits from screening.”
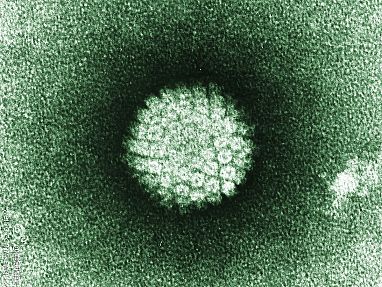
Electron microscope image of the human papillomavirus (HPV)
One of the most important challenges is determining the best way to manage someone’s health when they become infected with HPV, since only about a dozen of the roughly 200 strains of the virus cause cancer. Moreover, many HPV infections disappear by themselves within a couple years, giving in to the body’s immune attack with no outside help. Certain strains, however, such as HPV16 and HPV18, are more likely to persist, cause pre-cancerous changes to cells, and eventually lead to cancer.
“We’re trying to identify new biomarkers — that is, proteins or other molecules in the blood or cervical samples — that can predict risk,” Dr. Wentzensen says. “Then the translational piece is conducting large studies to evaluate the biomarkers to see how well they predict risk for pre-cancerous lesions and cancer development.” After that, organizations like the U.S. Preventive Services Task Force, the World Health Organization, and medical specialty societies can use that information to develop screening guidelines.
Those biomarkers include two molecules, p16 and Ki-67, that Dr. Wentzensen’s team has studied. The two molecules can be detected under a microscope in pre-cancerous and cancerous cervical cells using a ‘dual-stain’ approach, which causes them to become clearly visible in those cells because they each turn a specific color.
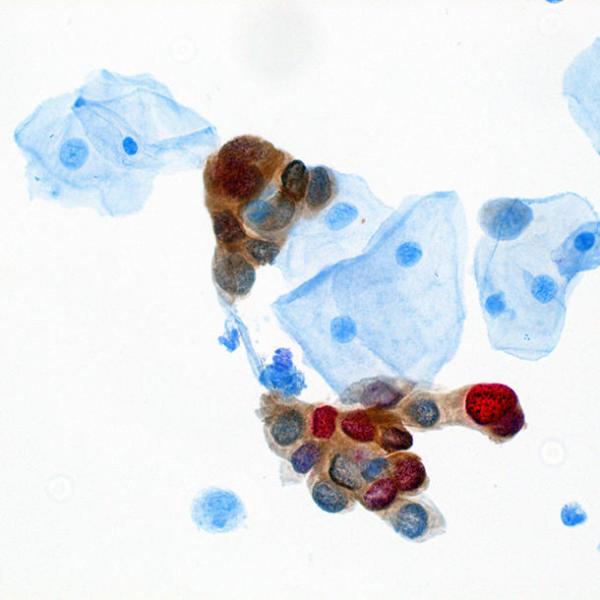
Dr. Wentzensen’s team uses a ‘dual-stain’ test to detect the presence of two proteins, p16 (brown) and Ki-67 (red).
Detecting p16 and Ki-67 is useful for the clinical management of HPV-positive women because the strains of HPV that cause cancer make two cancer-promoting ‘oncoproteins’ that interfere with the life cycles of infected cells. When the two oncoproteins throw their wrenches into the cellular machine, the p16 and Ki-67 proteins become highly abundant and therefore show up strongly on a microscope slide in the respective colors produced by the dual-stain test.
Unfortunately, just because the dual-stain test works well doesn’t mean it’s foolproof. Once the samples of cervical tissue are stained, an expert must still look at the cells and make a determination on whether the results indicate pre-cancer or cancer, which can sometimes be like finding a needle in a haystack.
“It’s much easier to pick out these two colors, but you still have to go through all of the cells on a slide,” Dr. Wentzensen explains. “It takes a while and there’s always a continuous range in how strongly the stains show up.”
However, artificial intelligence (AI) is helping to overcome this challenge. Dr. Wentzensen and his colleagues have developed and trained a prototype AI algorithm that can quickly review dual-stain test samples and detect cells that are positive for both p16 and Ki-67.1,2 The program not only enables clinicians to determine which samples contain pre-cancerous cells, but can also quantify the severity of the disease based on the number of positive cells in a sample.
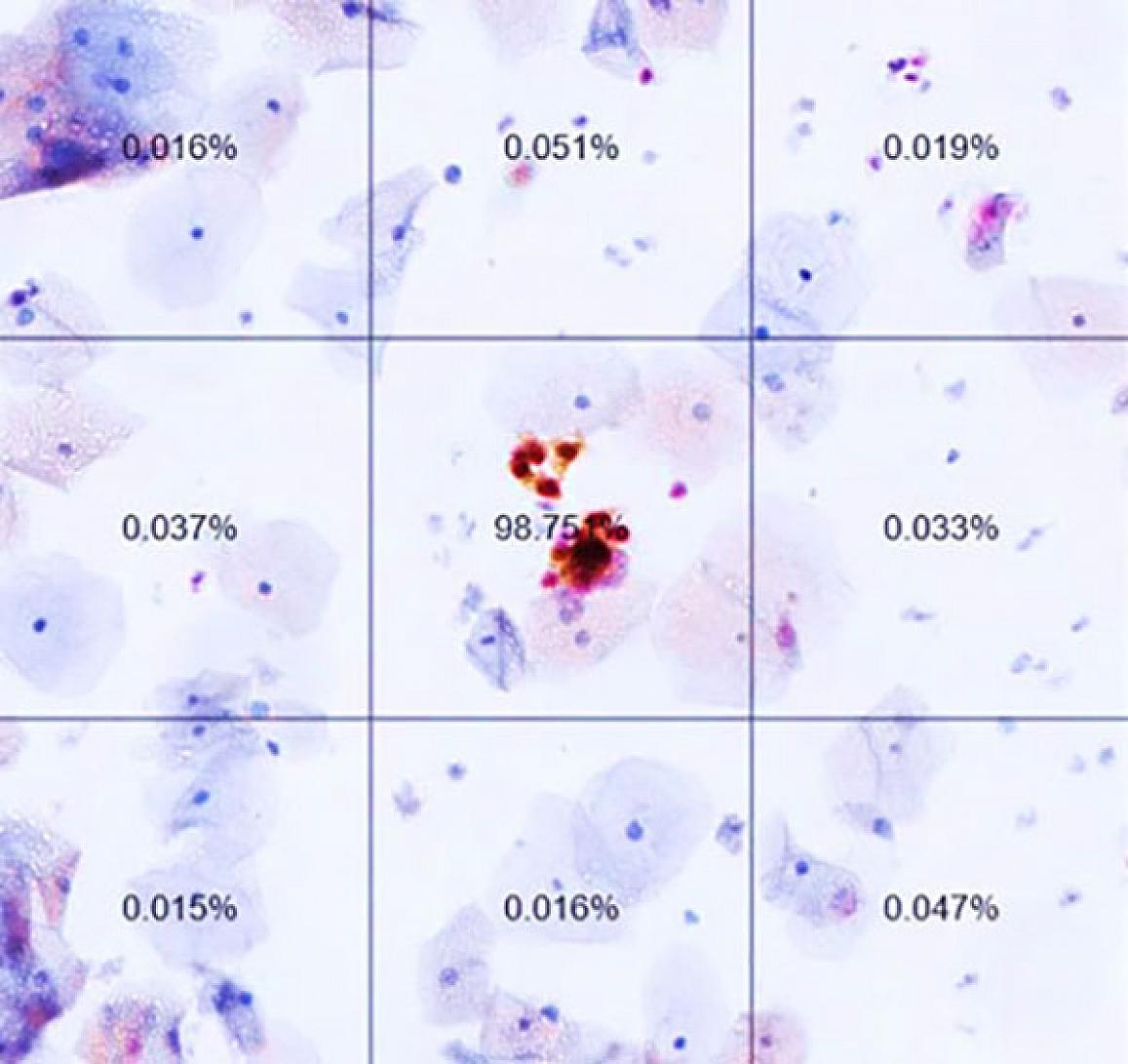
This slide from an automated dual-stain test performed using Dr. Wentzensen’s AI program, shows the likelihood that cervical cells are cancerous or pre-cancerous.
Now, Dr. Wentzensen’s team is figuring out how to translate the results of the AI software into clinical applications to decide when to conduct diagnostic evaluation and begin treatment. Working with multiple partners in the U.S. and Germany, including Kaiser Permanente Northern California and the University of Mississippi, Dr. Wentzensen and his collaborators have amassed thousands of samples from a wide variety of patients so they can put the AI screening test through its paces.

Dr. Nicolas Wentzensen
Moving forward, Dr. Wentzensen’s research group and his collaborators are continuing to search for and evaluate biomarkers in HPV-infected cells. At the same time, they’re looking for biomarkers that hint at the presence of HPV in other HPV-related cancers, such as anal cancer. What’s more, Dr. Wentzensen believes his team’s discoveries about cancers caused by HPV could have broader applications.3
“There are many parallels and many interesting applications for these markers and approaches, so I think we can use our experience and knowledge in other areas, not just in HPV-related cancers, but other gynecological cancers, such as endometrial cancers,” he says. “Just as HPV screening followed by biomarker testing has changed the landscape for cervical cancer, applying a similar research approach to other cancers and other biomarkers may make a huge difference.”
Check out this blog for another example of how IRP researchers have leveraged AI in the fight against cervical cancer, and subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Grabe N, Lahrmann B, Pommerencke T, von Knebel Doeberitz M, Reuschenbach M, Wentzensen N. A virtual microscopy system to scan, evaluate and archive biomarker enhanced cervical cytology slides. Cell Oncol. 2010;32(1-2):109-19. doi: 10.3233/CLO-2009-0508.
[2] Wentzensen N, Lahrmann B, Clarke MA, Kinney W, Tokugawa D, Poitras N, Locke A, Bartels L, Krauthoff A, Walker J, Zuna R, Grewal KK, Goldhoff PE, Kingery JD, Castle PE, Schiffman M, Lorey TS, Grabe N. Accuracy and Efficiency of Deep-Learning-Based Automation of Dual Stain Cytology in Cervical Cancer Screening. J Natl Cancer Inst. 2021 Jan 4;113(1):72-79. doi: 10.1093/jnci/djaa066. PMID: 32584382; PMCID: PMC7781458.
[3] Cohen CM, Wentzensen N, Lahrmann B, Tokugawa D, Poitras N, Bartels L, Krauthoff A, Keil A, Miranda F, Castle PE, Lorey T, Hare B, Darragh TM, Grabe N, Clarke MA. Automated Evaluation of p16/Ki-67 Dual-Stain Cytology as a Biomarker for Detection of Anal Precancer in Men Who Have Sex With Men and Are Living With Human Immunodeficiency Virus. Clin Infect Dis. 2022 Oct 29;75(9):1565-1572. doi: 10.1093/cid/ciac211.
Related Blog Posts
This page was last updated on Wednesday, February 19, 2025
