Applying Rare Disease Discoveries to Diabetes
Patients With Rare Metabolic Conditions Yield Insights Into Common Ailments

Studying rare diseases that affect the body’s fat stores and ability to process energy could help improve treatment for patients with obesity and type 2 diabetes.
Young doctors are taught the adage, “When you hear hoofbeats, think horses, not zebras.” Just as you would not expect to find a zebra in your barn, when making a diagnosis, you generally don’t expect to find an unusual disease. However, just as there are still zebras in the world, there are also rare diseases. On Rare Disease Day, celebrated on the last day of February each year, we call attention to the 300 million people affected by them.
Defined as conditions that affect fewer than 1 in 2,000 people, rare diseases pose both challenges and opportunities to medical research. Because they are so uncommon, diagnosis can take years, and treatments may be difficult to obtain or may not yet exist. However, for IRP Lasker Clinical Research Scholar Rebecca J. Brown, M.D., M.H.Sc., the study of several rare metabolic diseases may shed light on the causes of one of the most common diseases in the U.S.
“We hope we can use what we learn from the rare conditions to actually identify pathways that are targets for treatment of the more common conditions like type 2 diabetes,” Dr. Brown says.
Type 2 diabetes, which affects more than 28 million people in the U.S., develops when the body becomes resistant to the hormone insulin. Insulin is vital to our survival because it regulates blood sugar levels and feeds our cells. Like Goldilocks choosing between hot and cold porridge, we can’t have too much or too little sugar in our blood to maintain good health. As cells stop recognizing and using insulin, sugar accumulates in the blood, leading to serious immediate and long-term complications.

Because their bodies are insulin-resistant, people with type 2 diabetes must regularly measure their blood sugar levels to keep them from getting too high or too low.
Dr. Brown studies rare diseases that cause insulin resistance, mess with the function of insulin receptors, and disrupt insulin’s signals in the body. Among patients with these conditions, finding the root of the problem may be less complicated because there may be only a single genetic mutation responsible or the more pronounced nature of the disease makes the abnormal functioning easier to identify.
One disease Dr. Brown studies is generalized lipodystrophy, which prevents the body from storing fat. While that may sound like a dream to many of us, it’s a serious illness that can lead to severe metabolic disorders, which interfere with the body’s ability to harness energy from food, as well as heart disease and psychological distress due to the disease’s effects on how patients’ bodies look. It affects about 1 in 10 million people across the globe.
“We tend to think of fat as being harmful, but in fact, it has very important biological functions,” Dr. Brown says. “Not having fat in your body is actually just as bad, or even worse, for your health than having too much fat in your body. It turns out that the health complications of lipodystrophy are very similar to those of obesity.”
Fat stores excess nutrients to feed our bodies between meals and overnight in the short-term, and as a hedge against starvation in times of food scarcity. When nutrients flow into our fat depots, they expand by filling up existing fat cells and creating new ones. That’s fine up to a point, but once we reach a certain limit, problems can arise. When too much fat builds up in the muscles or liver, for instance, it can cause them to become insulin-resistant, interfering with insulin’s ability to deliver energy to their cells and harming their functioning. The rates at which the body’s various fat depots expand vary from person to person, so the point at which insulin resistance develops can vary. That’s why some people develop type 2 diabetes even with low levels of body fat, while others can gain a lot of weight and not develop diabetes.
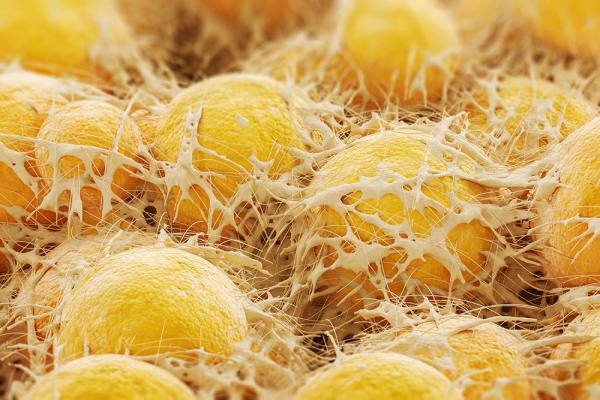
Human fat cells, known as adipocytes, as seen under a high-powered microscope.
“Lipodystrophy is like an extreme variant of a limited ability to expand fat, so I think it can help us understand the common biology underlying insulin resistance in both obesity and the rare condition of lipodystrophy,” Dr. Brown says. “If we were able to expand healthy fat storage in people with lipodystrophy, we likewise may be able to expand healthy fat storage in people with obesity.”
Dr. Brown also studies people who have genetic disorders or autoimmune diseases that damage or block insulin receptors, the cellular guards that allow blood sugar into cells. By comparing these patients to those with more common forms of insulin resistance, like those related to obesity, it is possible to understand what insulin does inside the cell and how both excess and insufficient insulin signals contribute to health problems linked to type 2 diabetes and obesity.
“Normally, you can only gain this kind of insight using mice, but we can learn about what’s happening in humans,” Dr. Brown says, “and we’re always looking for therapies for these diseases as well. “
One such therapy works by leveraging leptin, a hormone produced by fat cells. Since some patients with lipodystrophy are missing nearly all the fat in their bodies, they also have very low levels of leptin, so replacing the hormone can help alleviate their symptoms. However, it’s not a particularly effective treatment for people with a more common form of the disease that causes them to lack fat only in specific parts of the body, and it certainly doesn’t cure the disease in either group.

Dr. Rebecca Brown
“While I’m collaborating with investigators who are exploring gene therapy approaches, in my lab, we’re thinking of more pharmacological approaches,” Dr. Brown says. “One of the first steps is to determine if there are any precursors for fat cells inside the body that could potentially be stimulated to grow.”
To find out, Dr. Brown and her research team are looking at tissue biopsies for evidence of immature cell types that can turn into fat cells.
“Once we get past that initial stage, we hope to give drugs that may increase storage of fat in fat-deficient areas,” Dr. Brown says. “There are already drugs available that have potential to increase fat storage capacity, but we need to test how well they work.”
If any organization is set up to find an answer, it’s the NIH Intramural Research Program, Dr. Brown notes.
“Our patient care unit is specially designed to understand metabolism and conduct very complicated metabolic studies in patients,” she says. “I think the really unique aspect of NIH is that we have an entire hospital and Clinical Center that has as its major purpose conducting research.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
Related Blog Posts
This page was last updated on Thursday, February 29, 2024
