IRP’s Michael Chiang Elected to National Academy of Medicine
NEI Director is Envisioning the Future of Eye Research

Dr. Michael Chiang was elected to the National Academy of Medicine in October for his implementation of new technologies to improve the diagnosis and treatment of vision diseases.
Vision is one of the most important ways we experience the world around us, so naturally, when disease and injury threaten sight, the impact of that loss can cause significant harm to our quality of life. That’s why, when Michael F. Chiang, M.D., became director of NIH’s National Eye Institute (NEI), he felt it was so important to incorporate this sentiment into his Institute’s new mission statement: “To eliminate vision loss and improve quality of life through vision research.”
This past fall, Dr. Chiang was elected to the National Academy of Medicine (NAM) for his own contributions to that mission, through his research on eye disease and the use of data and technology to improve treatment and access to vision care. His work has particularly focused on the diagnosis and treatment of retinopathy of prematurity (ROP), a complication that can lead to blindness among premature and low-birthweight babies.
“It was an incredible honor,” Dr. Chiang says of his election to the NAM. “I used to read about the new members elected every year and view them as leaders and giants in the field of biomedical science. I honestly never envisioned that I would be considered for that group.”
Growing up, Dr. Chiang always assumed he would follow his family members into engineering. As an undergraduate, he held engineering internships at companies and laboratories that specialized in technologies for use in health care, including writing computer programs to analyze ultrasound images used to diagnose heart disease.
“The interplay between the technology and medicine — that you can build a machine and use it to take care of somebody — fascinated me,” Dr. Chiang says. “That’s what made me want to become a physician.”
Dr. Chiang’s path to eventually studying vision first passed through the field of ‘computational neuroscience’ via the division of neurosurgery research at Massachusetts General Hospital, where he worked under Richard Masland, Ph.D., studying the electrical properties and anatomy of neurons. The experience taught him a lot about the biological mechanisms behind vision, which depends on electrical signals sent from the eyes to the brain. As a result, he decided to focus on ophthalmology, the field of medicine particularly concerned with vision and eye health.
Vision depends on electrical signals sent from the eye to the brain along the optic nerve.
As someone who “likes to solve big problems,” when Dr. Chiang began his stint as a medical resident in ophthalmology in the late 1990s, he was inspired to address what was then a major hurdle in medicine. At that time, patient data came in the form of handwritten doctors’ notes and x-ray films posted against light boards, and he thought there was “surely a better way to manage that data” using emerging technologies like the Internet and the huge sets of patient data that researchers were beginning to collect. Subsequently, as a faculty member at Columbia University, Dr. Chiang used his background in engineering and biomedical informatics to address significant inefficiencies and variability in the way doctors diagnosed infants with ROP.
That disease, which occurs when abnormal blood vessels grow across the retina, is a leading cause of childhood blindness in the U.S. and worldwide, particularly among traditionally underserved populations. The severity of ROP varies from mild cases that heal on their own to serious cases that cause blindness, so diagnosing it and determining its stage of advancement is vital to initiating appropriate treatment. Traditionally, diagnosis requires an in-person consultation and depends on the subjective interpretations of each ophthalmologist.
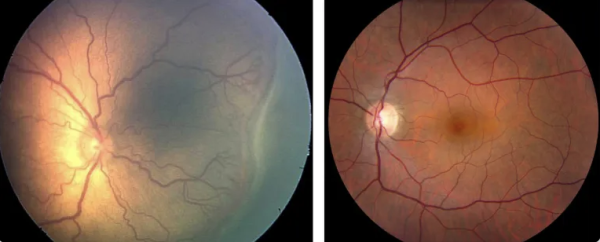
Left: Image of a premature infant’s retina showing signs of severe ROP with large, twisted blood vessels; Right: a healthy infant's retina. Image credit: Casey Eye Institute, Oregon Health and Science University, Portland, and National Eye Institute
As part of a research team at Columbia, his first big project was to help develop a telemedicine program for diagnosing ROP. The group trained nurses to take photographs of babies’ retinas and then studied whether doctors could make accurate diagnoses using those images, if the program was cost-effective, and whether families were comfortable with it. Telemedicine examinations of this sort are now considered acceptable as part of the standard of care for ROP.
In addition to improving the accessibility and efficiency of diagnosing ROP, Dr. Chiang and his colleagues explored ways to use artificial intelligence (AI) to improve the quality of clinical diagnoses.
“After working on imaging for ROP for so many years, I learned a lot about the limitations of clinical diagnosis,” he says. “Experts, when they review the same image, often come up with different diagnoses. Medical diagnosis overall is often very subjective and qualitative.”
To address that problem, Dr. Chiang and his scientific collaborators built one of the earliest ‘deep learning’ systems for clinical diagnosis, in which computers are programed to learn to recognize complex patterns using text, images, and other information. The technology received FDA breakthrough status in 2020, a designation that speeds up the approval of drugs and devices intended for serious conditions.
“Now, diagnosis is becoming more and more objective and quantitative because of advances in imaging and data science, and that has fundamentally changed the way that we think about diagnosing disease and taking care of patients,” Dr. Chiang says. “I'm proud that we worked on making a scientific discovery and translated that into real world practice.”

Dr. Chiang hopes the implementation of telemedicine technologies into vision care will help make that form of healthcare more accessible to traditionally underserved populations.
Now, as director of the NEI, Dr. Chiang prioritizes making advances in vision research accessible to everyone. When he led the Institute through revising its 50-year-old mission and strategic plan, diversity, equity, inclusion, and accessibility (DEIA) were considered integral.
“I would say that it was impressed upon me early in my career about the impact of health disparities on disease because I happened to study a disease that, unfortunately, disproportionately affects families that don’t receive good prenatal care,” Dr. Chiang says. “Furthermore, how can we emphasize the ‘A’ at the end of 'DEIA' to take more of a leadership role in developing technologies to improve accessibility and help develop best practices that help people navigate the world more easily? That’s one of the reasons that health disparities is one of the seven areas of emphasis in our strategic plan.”
After all, he adds, “We’re very proud of doing the best science in the world, but the best science in the world isn't nearly as useful if it's not available to the people, particularly those who need it the most.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
Related Blog Posts
This page was last updated on Wednesday, January 17, 2024
