Leveraging Turncoat Immune Cells to Combat Cancer
IRP Researchers Develop Drug to Recapture Immune Cells Hijacked by Tumors
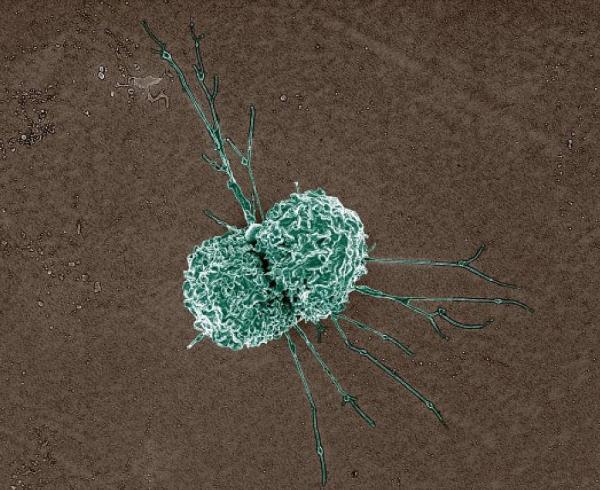
Macrophages like this one are supposed to help fight cancer, but tumors can convince them to switch sides. IRP researchers are working on a new cancer immunotherapy that works by reversing that process.
In the 1958 cult classic The Blob, a giant gelatinous creature from outer space lands on Earth and begins engulfing a small town and everything in it. While that may sound far out, a similar entity within our bodies does much the same thing, but for good instead of ill. These Pac-Man-like blobs are called macrophages — Greek for ‘big eaters’ — and they serve a vital role in keeping us healthy by clearing away dead cells and digesting foreign invaders like bacteria and cancer cells.
However, cancer cells aren’t content to just let themselves be eaten. They have evolved ways to overwhelm and commandeer the immune system, redirecting immune cells to support tumor growth rather than suppress it. Although highly personalized ‘immunotherapies’ that reboot the immune response and harness it to fight cancer have made significant advances in treating some forms of the disease, most cancers do not respond to these treatments. Fortunately, reinforcements are on the way: IRP senior investigators Udo Rudloff, M.D., Ph.D., and Juan Marugan, Ph.D., have identified a way to reclaim the loyalty of macrophages that are aiding and abetting tumors, turning them back into the cancer-consuming gluttons they were meant to be.1 Importantly, this approach may be effective on a broader array of cancers than other immunotherapies.
“Initially, immunotherapy was all about immune cells such as T cells,” says Dr. Rudloff, “but in the last decade people have recognized that other cells, like these macrophages, can be very helpful as well.”
Macrophages have a receptor molecule on their surfaces called CD206 that activates a process called phagocytosis — more Greek, in this case for ‘eating cells.’ When CD206 is triggered, macrophages catch and bind to foreign invaders and then push them inside themselves to be digested. At the same time, the activated macrophages send off chemical signals that tell other, ‘adaptive’ immune cells, such as T cells, to memorize the identity of the intruder and build up the body’s defenses against it.
Unfortunately, CD206 is a double-edged sword. Cancer cells can fight back against approaching macrophages by switching the receptor off, allowing them to hijack the macrophages and other cells to support the tumor’s growth. These tiny prisoners are called tumor-associated macrophages.

After being treated with a CD206 activator, this tumor-associated macrophage (outlined in red) engulfed a pancreatic cancer cell.
Once Dr. Rudloff and his team had mapped out how this happens, they began looking for a molecule that could selectively target CD206 receptors on tumor-associated macrophages and change the environment around the tumor in a way that would spur them to turn on their cancerous captors. For this, he turned to his friend and colleague, Dr. Marugan.
Together, they searched a library of molecules at NIH’s National Center for Advancing Translational Sciences (NCATS) for candidates with shapes similar to those of molecules that normally trip the CD206 switch. Using computer simulations, they found several candidates that met this criterion. Once they had winnowed the candidate molecules down to a small set, they chose one to try in animal models to evaluate how well it worked and how long it lasted in the body before being broken down.
“We were able to find molecules that worked very efficiently doing the same thing that the CD206 receptor did: activate the immune system and change the immune environment to suppress the growth of all kinds of tumors,” says Dr. Marugan. “This will be a new modality of immunotherapy using a small molecule.”
“A lot of immunotherapies are based on monoclonal antibodies, which are very large molecules,” adds Dr. Rudloff. “Ours is a small molecule that can penetrate the tumor and might ultimately be the better candidate for immunotherapy.”

Dr. Juan Marugan
One exciting aspect of this potential new treatment is that it seems to be ‘tumor agnostic,’ meaning it could be effective against any tumor that shows a high level of tumor-associated macrophages with CD206 receptors. Right now, the scientists’ animal and cell experiments are showing the treatment to be particularly potent against cancers of the pancreas, colon, and breast, as well as the skin cancer melanoma and the bone cancer osteosarcoma.
The IRP duo is now in the last stages of testing the new treatment and looking for a pharmaceutical industry partner that can help move it through the Food and Drug Administration’s regulatory processes and begin first-in-class human clinical trials for cancer. In addition, there is evidence that reprogramming macrophages that have been altered by disease can work in other conditions as well. Dr. Rudloff and Dr. Marugan are currently working with investigators in Japan who are developing a potential therapy for diabetic retinopathy, a complication of diabetes that can cause blindness and in which macrophages with the CD206 receptor play an important role.

Dr. Udo Rudloff
Of course, in addition to working with the pharmaceutical industry and their collaborators at universities around the world, Dr. Rudloff and Dr. Marugan have collaborated extensively with their colleagues in the IRP. They are quick to credit the team spirit and wealth of expertise available on the NIH campus for their success in translating their discoveries into a potential cancer therapy.
“As a physician-scientist, I cannot over-emphasize the importance of NCATS’ experts in medicinal chemistry, pharmacology, and biology,” says Dr. Rudloff. “We had this exciting mechanism, but it’s a big step to bring it to patients. You need to actually have a pill or an injection for patients to take.”
“Translation is always a team sport,” adds Dr. Marugan. “You need people with different kinds of expertise for each step. It’s a long-term relay race with different people taking the baton.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
Jaynes JM, Sable R, Ronzetti M, Bautista W, Knotts Z, Abisoye-Ogunniyan A, Li D, Calvo R, Dashnyam M, Singh A, Guerin T, White J, Ravichandran S, Kumar P, Talsania K, Chen V, Ghebremedhin A, Karanam B, Bin Salam A, Amin R, Odzorig T, Aiken T, Nguyen V, Bian Y, Zarif JC, de Groot AE, Mehta M, Fan L, Hu X, Simeonov A, Pate N, Abu-Asab M, Ferrer M, Southall N, Ock CY, Zhao Y, Lopez H, Kozlov S, de Val N, Yates CC, Baljinnyam B, Marugan J, Rudloff U. 202). Mannose receptor (CD206) activation in tumor-associated macrophages enhances adaptive and innate antitumor immune responses. Sci Transl Med. 2020 Feb 12;12(530). doi: 10.1126/scitranslmed.aax6337.
Related Blog Posts
This page was last updated on Tuesday, May 23, 2023
