New Treatment Creates Unwelcome Environment for Breast Cancer
Modifying Tumor’s Surroundings Stymies Cancer’s Expansion
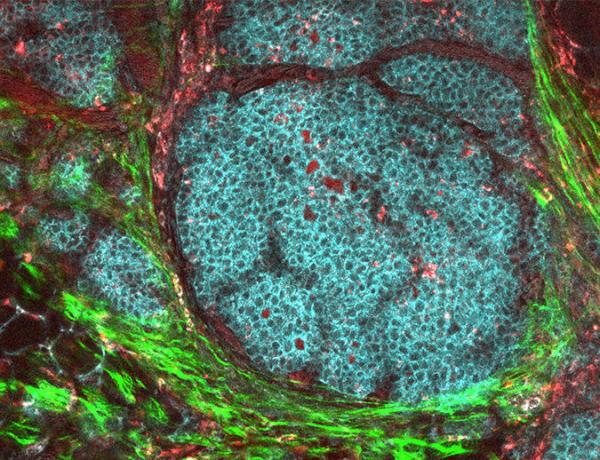
Breast cancer cells (blue) are able to spread to other parts of the body by altering their immediate surroundings and the environment at those other sites, but IRP researchers recently identified a promising method to stop this from happening. Photo credit: National Cancer Institute/Carbone Cancer Center at the University of Wisconsin
If you ever tried planting an apple tree in the desert or growing avocados in New England, you would quickly figure out that such plants need a particular environment in order to thrive. Cancerous tumors are no different, and IRP researchers recently found strong evidence that a molecule naturally produced in the body can suppress the growth and spread of a particularly lethal form of breast cancer via both direct effects on the cancer and by altering its surroundings.1
The main reason that cancer patients are more likely to survive if their disease is discovered early is that younger tumors are less likely to have spread from the site where they originated to other parts of the body. Numerous studies have shown that this process, called metastasis, depends on a tumor’s ability to alter the three-dimensional network of molecules that surround cells in our organs, known as the extracellular matrix. This cellular scaffolding acts like the soil in which a plant grows, providing both structural support and life-sustaining resources.
Evidence suggests that tumors can not only modify the extracellular matrix around themselves but also alter it in distant parts of the body to create a more welcoming environment for cancer cells, much like a mother bird prepares a nest for her eggs. This has prompted researchers like IRP senior investigator William Stetler-Stevenson, M.D., Ph.D., the new study’s senior author, to search for potential cancer treatments among molecules the body uses to regulate changes to the extracellular matrix. One such molecule is TIMP-2, which Dr. Stetler-Stevenson’s IRP lab discovered in 19892 and recently figured out how to produce in large enough quantities to administer as a potential therapy.3
“The site where metastasis occurs is prepared by the tumor to receive the cancer cells, and that involves changes in the extracellular matrix,” Dr. Stetler-Stevenson says. “Our approach is different from conventional cancer therapy in that it’s targeting the extracellular matrix as opposed to the cancer cells themselves.”
In the new study, Dr. Stetler-Stevenson’s team, including the study’s first author, David Peeney, Ph.D., examined how TIMP-2 affected a type of cancer called triple-negative breast cancer (TNBC). This cancer is particularly lethal because it spreads from the breast to other organs very quickly and is unaffected by many therapies that are effective against other forms of breast cancer. The IRP researchers found that giving TIMP-2 daily for three weeks to mice with TNBC tumors not only inhibited the growth of the tumor at the location where it was implanted in the animals’ breast tissue, but also reduced the number of TNBC cells in the animals’ lungs by more than 90 percent compared to untreated mice. Moreover, TIMP-2 did not cause any detectable side effects.

Dr. William Stetler-Stevenson
Further experiments showed that TIMP-2’s beneficial effects stemmed from its ability to stop the animals’ tumors from modifying themselves and their surroundings in a manner that would facilitate metastasis. For example, TNBC is normally able to metastasize by adopting the traits of so-called ‘mesenchymal’ cells that are able to move through the body, but TIMP-2 inhibited that process. Moreover, the spreading of a cancer to distant tissue is normally associated with changes to an extracellular matrix protein called periostin at that location, but these changes did not occur in mice treated with TIMP-2.
“Normally, there is an increase in periostin in the lungs prior to metastasis formation,” explains Dr. Stetler-Stevenson. “The actual function of it is not really that well-defined, but it’s an extracellular matrix component that tells you this is where metastasis may occur, and with TIMP-2 treatment we didn’t see that.”
Finally, the researchers found that lung tissue that had not yet been affected by the cancer showed changes in gene activity that inhibited the cancer’s growth in the lungs. What’s more, these changes were still apparent in the lungs two weeks after the researchers stopped giving the mice TIMP-2.
While previous studies have shown that TIMP-2 treatment can inhibit the growth of a tumor, Dr. Stetler-Stevenson’s new study is the first to demonstrate that TIMP-2 can reduce metastasis by altering the extracellular matrix in a way that makes distant sites like the lungs a less hospitable environment for cancer cells. The IRP team now plans to examine the effects of TIMP-2 in other animal models of cancer, as well as refine their treatment delivery method and modify the TIMP-2 molecule itself in order to make it more therapeutically effective.
“TIMP-2 could work in tandem with more classical chemotherapies or next-generation immunotherapies that promote tumor cell destruction but don’t normalize the surrounding tissue,” says Dr. Peeney. “TIMP-2 can restore a healthier extracelluar matrix to better allow patients to recover.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] TIMP-2 suppresses tumor growth and metastasis in murine model of triple-negative breast cancer. Peeney D, Jensen SM, Castro NP, Kumar S, Noonan S, Handler C, Kuznetsov A, Shih J, Tran AD, Salomon DS, Stetler-Stevenson WG. Carcinogenesis. 2019 Oct 17. pii: bgz172. doi: 10.1093/carcin/bgz172.
[2] Tissue inhibitor of metalloproteinase (TIMP-2). A new member of the metalloproteinase inhibitor family. Stetler-Stevenson WG, Krutzsch HC, Liotta LA. J Biol Chem. 1989 Oct 15;264(29):17374-8.
[3] Tissue Inhibitor of Metalloprotease-2 (TIMP-2): Bioprocess Development, Physicochemical, Biochemical, and Biological Characterization of Highly Expressed Recombinant Protein. Chowdhury A, Brinson R, Wei B, Stetler-Stevenson WG. Biochemistry. 2017 Dec 12;56(49):6423-6433. doi: 10.1021/acs.biochem.7b00700.
Related Blog Posts
This page was last updated on Tuesday, May 23, 2023
