Yoga Helps Pain and Brain
Five Questions with Dr. Catherine Bushnell
Yoga changes the physical structure of the brain in ways that may prove useful for patients with chronic pain.
Yoga is all the rage these days, with millions of people taking part in the practice for relaxation, meditation, and increasing flexibility and muscle strength. However, the benefits of yoga go beyond what most might think. In fact, the mind-body practice of yoga could have a significant impact on the lives of those living with chronic pain, a condition that affects tens of millions of Americans.
In the past, doctors often prescribed opioids to treat chronic pain. However, research has shown that people with chronic pain have anatomical and neurochemical alterations in the brain that make them less responsive to opioids. In addition, both the medical and political systems are currently contending with a public health crisis stemming from the over-use of opioid pain medications. As a result, researchers have been working to identify ways to better manage chronic pain, particularly without the use of medication.
In a 2013 study, researchers led by IRP senior investigator Catherine Bushnell, Ph.D., found that chronic pain and yoga have significant but opposite effects on the physical structure of the brain. In recognition of September as National Pain Awareness Month and National Yoga Month, I spoke with Dr. Bushnell about why she chose to study yoga, the connection between yoga and chronic pain, and how her research has influenced pain management practices.
Why did you choose to study yoga and the connection it could have to managing chronic pain?
“For the last 40 years, I’ve been interested in how psychological and environmental factors alter pain. We’ve found that attention, emotional state, and physical activity all have the ability to reduce pain. Yoga incorporates all of those factors, making it a particularly interesting mind-body technique.”
How has this research influenced thinking around chronic pain treatment?
“Over the years, we have seen that chronic pain is a huge problem. We’ve also seen that chronic pain is not always visible and is very different than acute pain. If I were to hit your finger with a hammer, you’re going to feel immediate pain, scream, and go ‘Ouch!’ However, someone with chronic pain can be in terrible pain and suffering deeply but not have that type of reaction. Through our research, we’ve found that chronic pain is real and can be seen through changes in the brain. It’s very important to treat this pain, but we also realize that treating pain with opioids can cause many, many problems.
“The research we’ve done shows that an individual, through his or her own means, can learn to engage the same networks in the brain that are engaged when taking a pain medication. Yoga is one of the ways a person can do this because it engages the parts of the brain that are important in dampening pain. This is done through the physical exercise, meditation, and breath control that yoga requires, which lead to the activation of areas of the brain which dampen pain, all without taking drugs.”
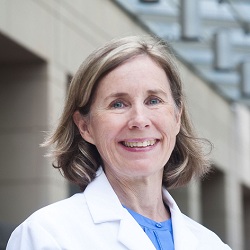
Dr. Catherine Bushnell
Were there any particular tools or collaborations that were important in conducting this research?
“One of the most important aspects of successfully completing this research was that one of my co-authors was a trained yoga instructor and had expertise in all factors important to yoga. I think that having a collaborator who was an expert in the technique was really important. In addition, it was essential to evaluate individuals’ pain, but it was also important to give people pain without actually harming them. We did this by using computer-controlled thermal stimuli, which allowed us to give people pain that we knew would be very brief, such as a burning sensation, and didn’t lead to any actual damage.”
What was the most challenging aspect of this study?
“This study examined people who practice yoga themselves, rather than assigning people to a yoga treatment or control group. Thus, we needed to find control subjects who matched the individuals being studied on factors other than yoga, such as age, sex, education level, and exercise outside of yoga. Since people who choose to practice yoga may have other characteristics in common, we needed to be certain that it was the yoga itself, and not other factors, that caused the effects we observed.”
How have you continued to study this topic, and what are your plans to study it in the future?
“After finishing this study we completed a follow-up study that examines the neurological benefits of yoga in further detail. As there are various types of yoga, we went on to look at how different aspects of yoga practices, including exercise, meditation, and breathing, contribute to changes in the brain and found that each of these aspects independently contributed to the increased gray matter — where the cell bodies of neurons reside — that we observed in the brains of yoga practitioners. Nevertheless, physical activity was the most important contributer to increased amounts of gray matter.
“In addition, we’re continuing to study the same concepts to further understand how to change pain without using drugs. Right now, we’re looking at non-invasive nerve stimulation as a way to manage pain, as well as using transcranial brain stimulation to affect the brain directly through the neural circuits that yoga engages to effectively manage pain.”
Head over to our Accomplishments page for more information on Dr. Bushnell’s research. You can also subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
Related Blog Posts
This page was last updated on Wednesday, May 24, 2023
