Cholesterol Molecule Yields Insights Into Distressed Lungs
Potential biomarker may contribute to personalized treatments
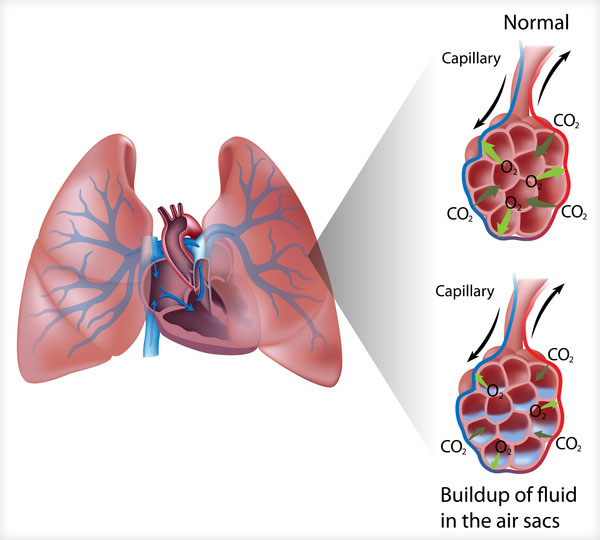
Acute respiratory distress syndrome (ARDS) occurs when fluid builds up in the lungs. New IRP research has identified a cholesterol-based molecule that appears to predict the severity of ARDS and may have implications for how the condition and other lung ailments are treated.
Until recently, medical treatment has largely been one-size-fits-all, with doctors unable to separate patients into distinct groups that might benefit more or less from a particular approach. However, researchers are increasingly finding that individuals with the same disease can differ markedly in ways that might one day influence their care. A recent IRP study has identified a particular molecule that may have just such an impact for patients with damaged lungs.1
The study’s senior author, IRP senior investigator Michael Fessler, M.D., initiated the research after reading a study published in 1999 that suggested immune cells in the lungs called alveolar macrophages produce large amounts of cholestenoic acid, a molecule made from cholesterol by essential cellular structures called mitochondria.2 Scientists believe that mitochondria synthesize cholestenoic acid so cells can release it into the bloodstream to prevent toxic cholesterol buildup inside them. As a result, Dr. Fessler wondered if lower levels of cholestenoic acid in the blood might signify that the mitochondria in alveolar macrophages — and thus the cells themselves — were not working correctly.
“Mitochondria need to be healthy in order to take in cholesterol for making cholestenoic acid,” explains Dr. Fessler. “If the mitochondria are unhealthy, this doesn’t happen, and you get less cholestenoic acid in the blood.”
To investigate his hypothesis, Dr. Fessler’s team first confirmed that alveolar macrophages from the lungs of healthy individuals showed high activity in a gene called CYP27A1 that is crucial to producing cholestenoic acid. Next, they examined levels of cholestenoic acid in blood from patients with an often lethal condition called acute respiratory distress syndrome (ARDS), which occurs when another ailment like a systemic infection or pneumonia causes an inflammatory reaction in the lungs. This allows fluid to leak into the lungs’ air sacs and makes it difficult to breathe. Dr. Fessler’s team found that ARDS patients with higher blood levels of cholestenoic acid were significantly less likely to die and also spent fewer days hooked up to a ventilator to help them breathe, a common intervention in severe cases of ARDS.
The researchers also examined the CYP27A1 gene’s activity in alveolar macrophages collected from a separate group of ARDS patients within two days of their diagnoses. Patients whose alveolar macrophages showed lower activity in that gene spent more days on a ventilator and had higher levels of inflammatory molecules in fluid collected from their lungs.
“One might wonder whether macrophages with deficient cholestenoic acid production — perhaps because of impaired mitochondrial function — are pro-inflammatory, which could drive lung disease,” says Dr. Fessler. “Or they might be less able to curb inflammation, since macrophages play a key role in resolving inflammation as well.”
Abnormal processing of cholesterol and other fat-based molecules in the lungs has been shown in a wide array of lung diseases,3 meaning Dr. Fessler’s findings could have implications not just for ARDS patients but for individuals with other lung ailments like chronic obstructive pulmonary disease (COPD) and asthma. Further examination of cholestenoic acid levels in those patient populations may eventually allow it to be used as a lung disease biomarker — a measurable indicator that reflects features of an individual’s health. Specifically, if blood levels of cholestenoic acid prove to reliably indicate poorly functioning alveolar macrophages, doctors might measure the molecule to inform their approach to treating ARDS and other lung diseases.
“The field is moving towards more personalized medicine,” says Dr. Fessler. “Eventually, we’re probably going to recognize that there are a bunch of different molecular pathways that can lead to the same lung syndromes, so if you could use biomarkers to identify the particular pathway by which a patient’s lungs were injured, perhaps you could give a tailored therapy specific to that type of patient.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Cholestenoic Acid is a Prognostic Biomarker in Acute Respiratory Distress Syndrome. Madenspacher JH, Stapleton RD, Suratt BT, Dixon AE, Lih FB, Lowe JM, Mould KJ, Janssen WJ, Morrell ED, Wurfel MM, Garantziotis S, Tomer KB, Fessler MB. J Allergy Clin Immunol. 2018 Oct 5. pii: S0091-6749(18)31368-X. doi: 10.1016/j.jaci.2018.09.017. [Epub ahead of print]
[2] Elimination of cholesterol as cholestenoic acid in human lung by sterol 27-hydroxylase: evidence that most of this steroid in the circulation is of pulmonary origin. Babiker A, Andersson O, Lindblom D, van der Linden J, Wiklund B, Lütjohann D, Diczfalusy U, Björkhem I. J Lipid Res. 1999 Aug;40(8):1417-1425.
[3] A New Frontier in Immunometabolism. Cholesterol in Lung Health and Disease. Fessler MB. Ann Am Thorac Soc. 2017 Nov;14(Supplement_5):S399-S405. doi: 10.1513/AnnalsATS.201702-136AW.
Related Blog Posts
This page was last updated on Tuesday, January 30, 2024
