Dysfunction in Janitorial Gene Contributes to ALS
IRP Study Points to Treatment Target for Fatal Neurological Disorder

New IRP research suggests a gene that helps cells dispose of malfunctioning proteins may play a key role in amyotrophic lateral sclerosis (ALS), a disease caused by the death of neurons that drive movement.
Just like we throw out our busted toasters and other appliances, our cells must continuously dispose of malfunctioning equipment to keep themselves working optimally. In certain neurological diseases, though, neurons die because they can’t get rid of misbehaving molecules. New IRP research provides crucial insights into a key player in this process, suggesting that restoring the function of a particular gene or boosting the levels of the enzyme it produces could help patients with the devastating disease known as amyotrophic lateral sclerosis (ALS).1
In people with ALS, the neurons that enable us to move around die, leading to movement problems and muscle weakness. Symptoms worsen over time and are ultimately fatal, as patients become unable to breath on their own.
“ALS is the most devastating neurodegenerative disease of all neurological diseases,” says IRP senior investigator Avindra Nath, M.D., the new study’s senior author. “It’s actually worse than cancer — 50 percent of patients will die within three years of diagnosis and 90 percent within five years — and, so far, there are really no good treatment options.”
An expert on viral infections of the nervous system, Dr. Nath has long been interested in ‘human endogenous retroviruses,’ segments of DNA in our genomes that were placed there by ancient viruses that infected our distant ancestors and persist to this day. Those DNA sequences make up as much as 8 percent of the human genome, and research by Dr. Nath’s lab and other groups suggests they may play a role in an array of diseases, including ALS.
"Those viral sequences in general are mostly silenced in adult cells, but in ALS and some other diseases, including many types of cancer, those endogenous retroviruses become active again,” explains former IRP postdoctoral fellow Marta Garcia-Montojo, Ph.D., the study’s first author. “We have seen that this hyperactivity can produce neurodegeneration, but we don’t know how.”

Even today, our DNA contains genetic material from viruses that infected our distant ancestors millions of years ago.
During her time in Dr. Nath’s lab, Dr. Garcia-Montojo scoured our DNA for specific sequences belonging to the HERV-K family of human endogenous retroviruses, particularly a subtype known as HML-2. One place she found HML-2 was in the middle of a gene called ASRGL1, which produces an enzyme of the same name. The ASRGL1 enzyme allows cells to get rid of proteins that malfunction when parts of them turn into chemicals called isoaspartates.
“These isoaspartates are degenerative — they are not good for the protein because where the isoaspartate forms, the protein starts to twist,” Dr. Garcia-Montojo says. “They produce kinks in the chain of the protein, so the protein starts to misfold. Proteins that misfold have to get degraded, but the problem with those proteins is that the isoaspartate is not recognized by the enzymes that degrade proteins. Since the proteins cannot get recognized, they cannot get degraded. And that’s the role of ASRGL1: it removes the isoaspartates so the protein can get degraded.”
In the new study, Dr. Garcia-Montojo and her colleagues in Dr. Nath’s lab studied the ASRGL1 gene’s links to ALS. They observed that the ASRGL1 gene was much less active in brain tissue from patients with ALS compared to healthy brain tissue. In addition, samples of brain tissue with less of the ASRGL1 enzyme tended to contain more neurons in which a protein called TDP-43 was hanging out in the cell’s cytoplasm rather than inside the nucleus, where it resides in healthy cells.
Because misshapen, malfunctioning TDP-43 tends to get stuck in the cytoplasm, and this phenomenon is a hallmark of ALS, the IRP team next examined the relationship between ASRGL1 and TDP-43. They found that TDP-43 and ASRGL1 interacted much more in neurons from healthy people than in those from ALS patients. What’s more, computer simulations showed that certain parts of TDP-43 have a tendency to turn into the isoaspartates that the ASRGL1 enzyme eliminates, suggesting that without ASRGL1 around, cells may not be able to get rid of dysfunctional TDP-43. Further bolstering this idea, suppressing ASRGL1 production in mice dramatically increased the number of neurons in their brains with TDP-43 in the cytoplasm instead of the nucleus and dramatically boosted the death of those cells.
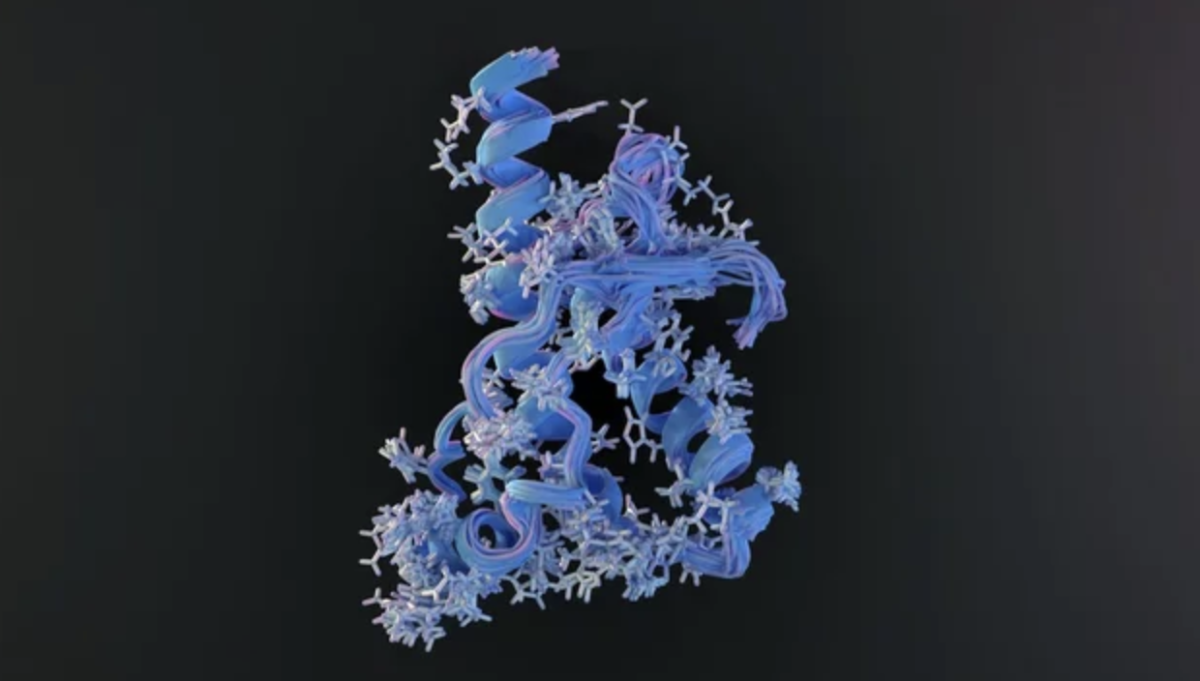
Without enough of the ASRGL1 enzyme, cells can’t get rid of misshapen proteins that aren’t working correctly, like the malfunctioning TDP-43 protein that is a hallmark of ALS.
Finally, the IRP scientists investigated the role that the viral HML-2 DNA might have in this process, since a copy of it exists within the ASRGL1 gene. They found that HML-2 was more active in brain tissue from ALS patients than tissue from healthy controls, and levels of the ASRGL1 enzyme plummeted when HML-2 activity was boosted in isolated neurons. The lack of ASRGL1, in turn, allowed misshapen TDP-43 to stick around in those neurons, which was fatal to them. However, restoring levels of the ASRGL1 enzyme kept those cells alive, which the scientists could accomplish by introducing extra copies of the ASRGL1 gene into the neurons or by suppressing the activity of HML-2. Ultimately, the IRP researchers hope that one of those two strategies might one day be used to save the lives of people with ALS.
"We have discovered, hopefully, a new therapeutic target for ALS, and now the next step will be how we can address the depletion of ASRGL1,” Dr. Garcia-Montojo says. One possibility could be introducing additional copies of the ASRGL1 gene into patients’ brains, possibly using a benign virus.

Dr. Nath (left), the study’s senior author, and Dr. Garcia-Montojo (right), the study’s first author
“The problem, of course, is how to get the DNA into the neuron,” she continues. “This is an issue that many research groups and companies are trying to address.”
Meanwhile, Dr. Nath’s lab continues to investigate the role of the ASRGL1 enzyme in ALS. His lab’s examination of brain tissue from patients suggests that HML-2 is not the only obstacle to ASRGL1’s ability to take out the trash inside neurons.
“What was interesting in this study is that we saw this depletion of ASRGL1 in the majority of the ALS patients, while we only saw HML-2 activation in a subset of about 30 percent, so it seems like this phenomenon of loss of ASRGL1 is much more prevalent than activation of HML-2,” Dr. Garcia-Montojo says. “Probably one of the causes of ASRGL1 depletion might be the over-activity of HML-2 in some patients, but there have to be other causes as well. It could be genetic mutations in ASRGL1 or associated genes. ASRGL1 is a new player in ALS and we still need to address many questions about its involvement in the disease.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Garcia-Montojo M, Fathi S, Rastegar C, Simula ER, Doucet-O'Hare T, Cheng YHH, Abrams RPM, Pasternack N, Malik N, Bachani M, Disanza B, Maric D, Lee MH, Wang H, Santamaria U, Li W, Sampson K, Lorenzo JR, Sanchez IE, Mezghrani A, Li Y, Sechi LA, Pineda S, Heiman M, Kellis M, Steiner J, Nath A. TDP-43 proteinopathy in ALS is triggered by loss of ASRGL1 and associated with HML-2 expression. Nat Commun. 2024 May 16;15(1):4163. doi: 10.1038/s41467-024-48488-7.
Related Blog Posts
This page was last updated on Tuesday, August 6, 2024
