Delivering on Maternal Health
IRP’s Katherine Grantz Develops Tools to Predict Pregnancy Complications

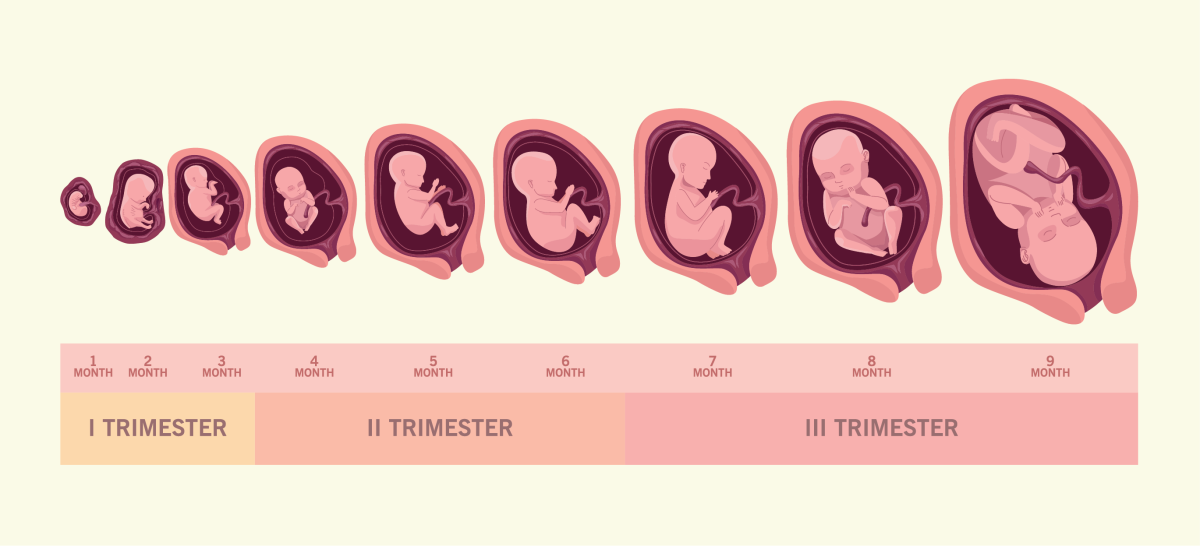
Fetal growth can indicate how well a pregnancy is progressing and help inform timing of delivery, making it a crucial indicator for the research of IRP senior investigator Katherine Grantz.
Advancements in medicine have reduced the risk of childbearing dramatically, but rates of maternal death have been creeping up in recent years. The reasons are varied. Older first-time parents, greater health concerns like obesity and hypertension, and lack of access to maternity care are important factors.
In observance of Maternal Health Awareness Day on January 23, we spoke with Katherine Grantz, M.D., a maternal-fetal medicine specialist and senior investigator at the Eunice Kennedy Shriver National Institute on Child Health and Human Development (NICHD). She is trying to improve health for pregnant people and their babies experiencing complications like gestational diabetes and hypertension, as well as reduce preterm deliveries and unnecessary C-sections.
“With increasing weight and maternal age, there’s a subsequent increase in a lot of pregnancy-related disease and pregnancy-specific complications,” says Dr. Grantz.
Fetal growth is an important indicator for how well a pregnancy is progressing and guides clinical management decisions from nutrition to disease treatment to determining the best time for delivery. A very small fetus may indicate health problems such as high blood pressure, malnutrition, or other complications that could result in a stillbirth or illness. Meanwhile, a very large fetus may indicate health problems for both mother and baby, such as gestational diabetes, and could lead to injuries at birth. Knowing what to expect helps medical professionals and expecting parents make appropriate choices and prepare for any complications during delivery and after.
“I'm very interested in the timing of delivery for pregnancy,” Dr. Grantz says. “Fetal growth is important in part, because it is related to timing of natural delivery and helps to inform delivery planning when the pregnancy is complicated by abnormal growth. Right now, there’s some debate over the optimal time to deliver these pregnancies for best results.”

Dr. Katherine Grantz
That’s because making that determination has always been more of an art than a science. Reliable, standard growth charts based on a large, diverse group of pregnant people didn’t exist for developing fetuses until 2015 when researchers at NICHD completed the first large-scale study of 2,334 pregnant women from diverse communities in the U.S.1,2 Before then, multiple charts based on small studies were available, but they varied among clinics, causing confusion. One clinic might determine a fetus is in the 9th percentile of growth, meaning it is undersized, and then refer the mother to a specialist where a different chart indicates the fetus is within the normal growth range.
Diversity was another issue with the older charts. The most common fetal growth reference used in the U.S. — the Hadlock reference — was based on a study of 392 Caucasian patients from Texas. In contrast, NICHD has conducted multiple sub-studies of women from multiple racial and ethnic backgrounds. This studies included women with complications like gestational diabetes and who gave birth to twins, which offers a more refined understanding of fetal growth among pregnancies.3
In addition to a more reliable and uniform growth chart, Dr. Grantz and her team has developed a second tool that helps determine how fast a fetus is growing, known as its 'fetal velocity.'
“It's typical to identify abnormal fetal growth using a one-time measurement,” Dr. Grantz says. “For example, if the estimated fetal weight is less than the 10th percentile, then the pregnancy might be flagged as undersized, or if it's greater than the 90th percentile, it can be flagged as being large for gestational age.”
The problem with using one measurement in time is that it can be difficult to distinguish between babies that are growing abnormally due to a health issue and babies that are healthy, but just happen to be bigger or smaller than average. Likewise, a single measurement can miss an abnormally growing fetus if it is on the borderline of what’s considered normal. However, if the rate of growth is slowing down or speeding up, doctors can determine if the size is truly indicative of a serious problem.
"Our studies suggest that if you add in velocity of fetal growth, it decreases the error in predicting birth weight,” Dr. Grantz says
Dr. Grantz’s research focuses on 'fetal velocity,' or how fast a fetus is growing, to identify pregnancies that might be at higher risk for health complications.
“I've always had a keen interest in providing data to fill in data gaps regarding clinical guidelines and obstetrics,” Dr. Grantz says of her work. In the past, pregnant people were often excluded from clinical trials and research due to safety concerns, but their omission came with the absence of data to guide clinical management. Now that the field is better balancing the risks of fetal harm with the potential health benefits to the mother and child, Dr. Grantz says they can begin to address many unanswered questions.
“Questions such as when to induce delivery in patients with high blood pressure or diabetes are common, but very challenging,” she adds. “That's what I'm trying to tackle: to see if we can provide data to help inform guidelines and answer these difficult-to-answer but important questions.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Grantz KL, Grewal J, Kim S, Grobman WA, Newman RB, Owen J, Sciscione A, Skupski D, Chien EK, Wing DA, Wapner RJ, Ranzini AC, Nageotte MP, Craigo S, Hinkle SN, D’Alton ME, He D, Tekola-Ayele F, Hediger ML, Buck Louis GM, Zhang C, Albert PS. Unified standard for fetal growth: the Eunice Kennedy Shriver National Institute of Child Health and Human Development Fetal Growth Studies. Am J Obstet Gynecol. 2022 Apr;226(4):576-587. doi: 10.1016/j.ajog.2021.12.006.
[2] Grantz KL, Grewal J, Kim S, Grobman WA, Newman RB, Owen J, Sciscione A, Skupski D, Chien EK, Wing DA, Wapner RJ, Ranzini AC, Nageotte MP, Craigo S, Hinkle SN, D'Alton ME, He D, Tekola-Ayele F, Hediger ML, Buck Louis GM, Zhang C, Albert PS. Unified standard for fetal growth velocity: the Eunice Kennedy Shriver National Institute of Child Health and Human Development Fetal Growth Studies.(external link) Am J Obstet Gynecol. 2022;227(6):916-922.e1.
[3] Grantz KL, Hediger ML, Liu D, Buck Louis GM. Fetal growth standards: the NICHD fetal growth study approach in context with INTERGROWTH-21st and the World Health Organization Multicentre Growth Reference Study. Am J Obstet Gynecol. 2018 Feb;218(2S):S641-S655. e28.2017.11.593. doi: 10.1016/j.ajog.
Related Blog Posts
This page was last updated on Tuesday, January 23, 2024
