Old Drugs Find New Potential Against Hepatitis C
IRP Research Highlights a Novel Target to Stop Viral Infections

Image credit: National Center for Advancing Translational Sciences
IRP researchers used specially designed robots to sift through more than 300,000 molecules for compounds that might be effective against the hepatitis C virus.
On July 28, health providers, researchers, patients, advocates, and governments across the globe observe World Hepatitis Day. Like this year’s theme, ‘Hepatitis Can’t Wait,’ IRP researchers are wasting no time utilizing the unique resources at the National Institutes of Health to identify innovative ways to combat the virus.
IRP Distinguished Investigator T. Jake Liang, M.D., for example, has focused his life’s work on understanding how hepatitis viruses infect, replicate, and persist in cells. The viruses he studies, hepatitis B and C, together affect more than 10 percent of the worlds’ population and are the most common causes of chronic liver disease and liver cancer. The two viruses were originally discovered in the 1980s by another IRP scientist, Harvey J. Alter, M.D., who shared the Nobel Prize in Medicine for that work in 2020. Nearly three decades later, Dr. Liang’s lab at the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) worked with scientists at the National Center for Advancing Translational Sciences (NCATS) to develop a novel test to screen thousands of molecules using a technology called high-throughput screening, which led to the discovery of several compounds with the potential to block hepatitis C infection.
“I was inspired by a presentation I attended, more than ten years ago, on how Viagra came to the market,” Dr. Liang explains, noting that the medication was originally developed to treat high blood pressure before being repurposed for erectile dysfunction. “That’s when I thought of this project to repurpose existing drugs for hepatitis C.”

More From the IRP
Blog
IRP’s Harvey Alter Awarded Nobel Prize
At the time, the only therapy for hepatitis C was a drug called interferon, which was only effective in about 20 percent of patients and came with harsh side effects. Pharmaceutical companies were focusing on various parts of the hepatitis C infection process and developing treatments to interfere with those steps, but Dr. Liang decided to take the opposite approach: find a compound that blocks viruses from infecting cells in petri dishes and then work backwards to understand how exactly it does that.
“It took a while, but fortunately, we were successful in developing a set of screening platforms for high-throughput screens of thousands of compounds very rapidly,” Dr. Liang says.
High-throughput screening uses robotics to combine and test vast sets of chemical compounds against a specific molecule or type of cell — in this case the hepatitis C virus — and search for interactions between them. The test Dr. Liang’s team and their NCATS collaborators developed led to the identification of several promising molecules, some of which had never been used for therapeutic purposes previously. Others belonged to a class of compounds previously approved for use as antihistamines, which reduce allergy symptoms like congestion and hives. The idea of repurposing those antihistamines for treating hepatitis C was attractive for several reasons.
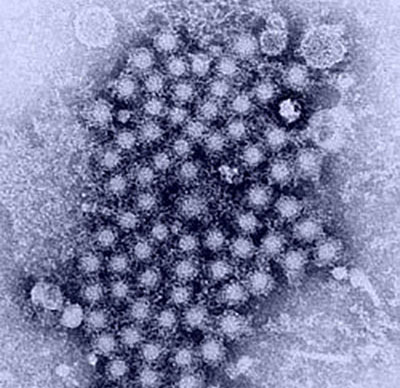
Image credit: U.S. Centers for Disease Control and Prevention
A cluster of hepatitis viruses, as seen through a transmission electron microscope.
“It takes a minimum of 10 years to get to a stage where a brand-new drug might show some kind of commercial benefit, and doing so can cost at least a billion dollars,” Dr. Liang says. On the other hand, by finding new uses for existing drugs, scientists can save that time and money while reducing the risks because they can proceed quicky to clinical trials as long as they stick to the approved dose.
There are drawbacks to this method, of course. Unless the pharmaceutical company is repurposing its own product, developers can run into patent issues. At the same time, the approved dose of a drug may not be high enough to alleviate the new condition.
That’s an issue Dr. Liang’s research team ran into with the antihistamine they selected for further study. Although laboratory studies showed a potent reaction between the drug and the hepatitis C virus, when tested at the approved dose in patients at the NIH Clinical Center, it didn’t block infection. The researchers solved this problem by modifying the molecule’s chemical structure with the addition of small groups of atoms, an alteration that made it more effective at blocking hepatitis C infection.
Meanwhile, Dr. Liang also needed to understand how the antihistamine was working to stop the virus.
“There are many steps you can interrupt in the infection process,” Dr. Liang says. “Most people target the machinery that allows the virus to replicate once it is inside the cell. We found this drug blocks the virus from getting into the cell before it has a chance to replicate.”
During the infection process, a virus attaches to the outside of a cell and then begins to fuse with the cell. This allows genetic material from the virus to enter the cell, where it hijacks the cell’s machinery and starts making copies of itself. The drug Dr. Liang’s lab focused on binds to the coating that surrounds the virus and prevents it from fusing with the cell.

Dr. T. Jake Liang
Since Dr. Liang published his findings in 2015 on the new and repurposed compounds his drug screen identified, an unrelated antiviral combination therapy was approved by the U.S. Food and Drug Administration in 2017. However, because the new therapy doesn’t work for everyone, he believes there may be room in the market for another treatment based on his discovery if a company wants to carry out clinical trials. In the meantime, his team’s discovery has important implications for both the value of repurposing drugs and the utility of a drug that interrupts fusion of a virus with a cell.
“These studies provided us with new, fundamental knowledge about viral infections specifically and biology in general,” says Dr. Liang. “When we studied the mechanism of the antihistamines and the other compounds that showed activity against hepatitis C, we found they were all targeting the same step of viral infection — that is, viral fusion.”
Having realized that the fusion process was common across all viruses, Dr. Liang’s team is now testing compounds that interrupt the process in other infections, including hepatitis B and COVID-19.
“We may be converging on an attractive concept of creating a broad-spectrum antiviral,” says Dr. Liang. “A certain compound may be active against many different classes of virus. These findings provided novel fundamental knowledge about the biology of viral infection that we may be able to leverage against other illnesses.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
Related Blog Posts
This page was last updated on Tuesday, May 23, 2023
