Simple Blood Test May Thwart a Complicated Cancer
Signs of Past Viral Exposure Predict Liver Cancer Risk

Looking for signs of past viral infections in patients’ blood could help doctors better predict their risk for developing liver cancer.
The liver has a difficult but important job. It serves as the central processing plant for all the food, drinks, and drugs we take in, separating and breaking them down into usable nutrients and toxic wastes that need to be removed from the body. It’s no surprise, then, that diseases affecting the liver can have life-threatening consequences. In particular, infections like hepatitis B and C and liver damage caused by alcohol, drugs, or fatty liver disease can all lead to liver cancer. Unfortunately, even though the presence of these conditions are harbingers of possible liver cancer, the disease often passes unnoticed until it is at an advanced, less treatable stage.
IRP senior investigator Xin Wei Wang, Ph.D., and his NIH research team are developing ways to detect liver cancers much earlier, when existing treatments are much more likely to stop their growth. In honor of Liver Cancer Awareness Month this October, I talked to Dr. Wang about his research and the novel blood test his lab has developed to predict liver cancer risk.
“The traditional approaches to assessing an individual’s risk for cancer, especially liver cancer, and for detecting it at an early stage are really sub-optimal,” Dr. Wang says. “The medical guidelines are to screen patients with chronic liver diseases every six months for evidence of tumor lesions in the liver, but the outcome is quite mixed. The majority of patients are still diagnosed at an advanced stage.”
There are a number of reasons regular screening for liver cancer has not been effective. For one thing, many patients don’t continue getting regular screenings, especially if their results look fine in the first few years. What’s more, current tests like ultrasound imaging and measurements of biomarkers that hint at the presence of a liver tumor aren’t refined enough to catch the disease in its early stages.
“The technology is getting better and better, allowing us to detect a tumor as small as one or two centimeters,” Dr. Wang says, “but even at this size, some tumors are already pretty aggressive. We think the cancer may actually occur years before symptoms or visible tumors appear.”
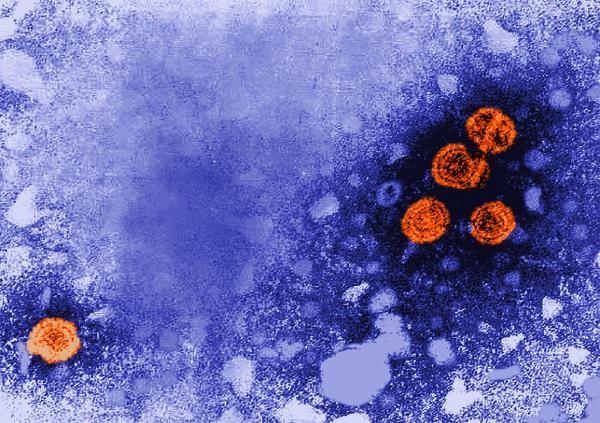
The hepatitis B virus (orange) is an underlying factor behind many cases of liver cancer.
The primary cause of the most common form of liver cancer, hepatocellular carcinoma (HCC), is thought to be the hepatitis B and C viruses. However, not all people infected with these viruses go on to develop HCC, and while vaccinations against hepatitis B and medications that inhibit hepatitis C have greatly reduced the prevalence of chronic hepatitis B and C infections, HCC rates have not dropped significantly. This may be partly due to the way viruses alter the body’s immune system, so people’s different responses to the hepatitis B and C viruses may influence their ultimate risk for HCC. While this seems to present a complication for predicting who will develop HCC, Dr. Wang and his colleagues suspected these different immune responses might create measurable biomarkers that could reveal patients’ risk for the cancer.
To test that idea, Dr. Wang’s laboratory ran tests on blood samples from 899 people enrolled in a long-term liver cancer study headed by the National Cancer Institute (NCI) and the University of Maryland. Using a new technology called VirScan, the researchers were able to compare blood samples from the patients against a library of 1,000 viral strains to detect which ones each patient had been previously exposed to, and of these, which were associated with HCC. By doing this, they discovered that past exposure to many different viruses other than hepatitis B and C was associated with higher HCC risk.1 What’s more, they were able to develop a simple blood test that can measure risk for developing HCC based on the presence of antibodies in people’s blood that their bodies produced during past viral infections.

Dr. Xin Wei Wang
While this study and a follow-up to confirm its results were both performed in relatively small populations, Dr. Wang says the data is encouraging enough that his team plans to try out the blood test in a population of 6,000 volunteers to see if it could be a viable tool for liver cancer surveillance and diagnosis. Based on their findings so far, the group believes their blood test can identify patients at high risk for HCC as early as seven years before they receive a diagnosis. If this turns out to be true, doctors could one day use the test to identify individuals who need to be closely monitored for the development of HCC so they can catch it and begin treatment as soon as the disease appears.
“I was surprised,” Dr. Wang said of the positive results. “We were able to identify many of the viral features that actually show an association with HCC and compare them to those not related to liver cancer. This was very exciting, because we didn’t really expect it.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Liu J, Tang W, Budhu A, Forgues M, Hernandez MO, Candia J, Kim Y, Bowman ED, Ambs S, Zhao Y, Tran B, Wu X, Koh C, Surana P, Liang TJ, Guarnera M, Mann D, Rajaure M, Greten TF, Wang Z, Yu H, Wang XW. (2020). A viral exposure signature defines early onset of hepatocellular carcinoma. Cell. 2020; Jul 23;182(2):317-328. doi: 10.1016/j.cell.2020.05.038.
Related Blog Posts
This page was last updated on Tuesday, May 23, 2023
