Collaboration Leads to Better Imaging
In NIDDK-NIBIB’s Biomedical and Metabolic Imaging Branch
In 2011, two NIH institutes joined forces to share their expertise and sophisticated imaging tools to advance the understanding of cardiovascular disease, diabetes, and other challenging health conditions. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the National Institute of Biomedical Imaging and Biomedical Engineering (NIBIB) have been running a joint operation called the Biomedical and Metabolic Imaging Branch (BMIB) in the heart of the NIH Clinical Center (Building 10).
“Our multidisciplinary team includes imaging physicists, spectroscopists, and clinicians,” said NIDDK senior radiologist Ahmed Gharib, who manages the daily operations of the branch. BMIB’s high-quality imaging capabilities provide basic scientists and clinicians with a more accurate depiction of a developing disease, while low-quality images increase the likelihood of misdiagnosis.
For example, a low-resolution liver scan may leave important details—such as tiny tumors–blurry and difficult to identify. High-resolution scans, taken from many angles, however, provide clear and detailed images that enable researchers to pinpoint problems earlier in a disease. Advanced imaging techniques can also be used to examine multiple organs simultaneously, making it possible to understand, detect, and manage various systemic diseases.
“Advances in imaging allow us to view parts of the body at a level of anatomic and functional detail and speed that had not been possible in the past,” said Gharib. BMIB researchers use a computed-tomography (CT) technique to capture crisp images of the heart’s blood vessels while the heart is beating. Imaging a moving heart is somewhat like photographing a fast-moving car—the more shots you take, the greater the likelihood that at least one will be clear. “We can now get a full cardiac CT in one to two heartbeats, compared [with] 16 [beats] just a decade ago,” Gharib explained. “This kind of development has made a big impact in translational biomedical research.”
Ahmed Gharib, NIDDK
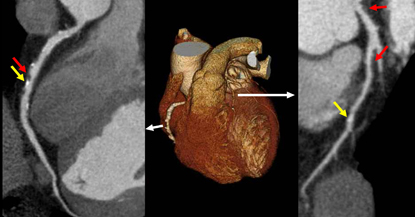
BMIB’s high-quality imaging capabilities provide basic scientists and clinicians with a more accurate depiction of a developing disease. Here, a Multidetector Computerized Tomography 3-D reconstructed image of the whole heart (center) is flanked by detailed images that were produced by a technique called multiplanar reformatting; the red arrows indicate non-calcified coronary plaques and the yellow arrows indicate calcified plaques: (right) right coronary artery; (left) left anterior descending coronary artery.
The BMIB’s use of state-of-the-art imaging equipment and newly developed techniques benefit a variety of patients and support an expansive range of research across NIH. Proton magnetic-resonance spectroscopy (MRS), for example, allows researchers to measure not only fat in the liver but also metabolites such as glycogen and choline (1). Studying these liver metabolites enhances the understanding of lipid and glucose metabolism under the more controlled environment of a metabolic unit.The BMIB grew out of NIDDK’s Integrated Cardiovascular Imaging Lab, which focused its efforts on demonstrating the link between metabolic syndrome (a combination of factors that increases the risk of heart disease, stroke, and diabetes) and atherogenesis (the formation of lesions in arterial walls). Today BMIB researchers work with the NIDDK-led Metabolic Clinical Research Unit (MCRU) to investigate the interrelationship between obesity, coronary heart disease, and other conditions. Obese MCRU patients often go to the BMIB to be scanned in its 3-tesla magnetic-resonance imaging (MRI) machine that can accommodate people who weigh up to 500 pounds. The imaging techniques used on such patients allow scientists to better understand a range of metabolic diseases.
“The work that we are doing in the branch holds tremendous promise for improved understanding of systemic disease and for early detection methods [especially for] atherosclerosis, which has long been the number one killer in much of the developed world,” said NIBIB Director Roderic Pettigrew. “We hope to see hospitals throughout the world one day using approaches based on this research.”
In keeping with NIH’s focus on collaboration, BMIB staff scientists Ronald Ouwerkerk and Khaled Abd-elmoniem and others work closely with other institutes—such as NICHD, NIAID, and NHLBI—that also depend on advanced imaging. For example, BMIB investigators have developed MRI and MRS techniques that can assess the metabolic composition of various organs and measure tissue stiffness (2). High-resolution coronary MRI provides a twofold improvement over conventional MRI in spatial resolution (3).
Additionally, improvements in temporal resolution allow researchers to view and measure the thickening of the coronary artery wall, the earliest stage of coronary artery disease (4). In the future, these new techniques may be used to monitor the effects of therapies and screen people at risk for coronary artery disease as well as metabolic and hepatic dysfunction.
“The collaborative infrastructure at NIH has enabled all of us to work together more efficiently,” said NIDDK Director Griffin P. Rodgers. “The Biomedical and Metabolic Imaging Branch is an excellent example of what can be accomplished through ongoing partnerships within NIH.”
For information on BMIB’s cardiac imaging service, go to http://intranet.cc.nih.gov/cardiacimaging/test.html (available to NIH staff only). Other NIH Catalyst articles on imaging appeared in the January-February 2009 issue and in the October 2009 issue.
References
- R. Ouwerkerk, R.I. Pettigrew, and A.M. Gharib, “Liver metabolite concentrations measured with 1H MR spectroscopy,” Radiology 265:565–575, 2012.
- D.A. Herzka, M.S. Kotys, R. Sinkus, R.I. Pettigrew, and A.M. Gharib, “Magnetic resonance elastography in the liver at 3 Tesla using a second harmonic approach,” Magn Reson Med 62:284–291, 2009.
- A.M. Gharib, K.Z. Abd-Elmoniem, V.B. Ho, et al., “The feasibility of 350 µm spatial resolution coronary magnetic resonance angiography at 3 T in humans,” Invest Radiol 47:339–345, 2012.
- K.Z. Abd-Elmoniem, A.M. Gharib, and R.I. Pettigrew, “Coronary vessel wall 3-T MR imaging with time-resolved acquisition of phase-sensitive dual inversion-recovery (TRAPD) technique: initial results in patients with risk factors for coronary artery disease,” Radiology 265:715–723, 2012.
This page was last updated on Thursday, April 28, 2022
