From the Annals of NIH HIstory
Where Did All the Acne Go?
Gary Peck’s Discovery Led to a Drug to Treat Severe Acne
BY E. GORDON MARGOLIN, OFFICE OF NIH HISTORY
Did you know that an NIH scientist’s work on a vitamin A derivative (retinoid) led to the development of a drug that can treat, and even cure, severe acne? Acne affects up to 50 million Americans annually; 85% of people between the ages of 12 and 24 have experienced at least minor acne, according to the American Academy of Dermatology. Most cases are mild and may be controlled with topical therapy. But about 15% of cases are severe enough to cause scarring and won’t respond to antibiotics and other conventional therapies. NIH’s Gary Peck discovered, in the 1970s, that a powerful drug called isotretinoin (or 13-cis retinoic acid) was effective against treatment-resistant severe acne.
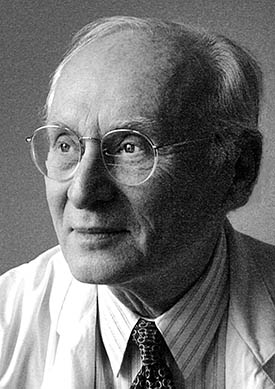
COURTESY OF GARY PECK
In the 1970s, NCI Senior Investigator Gary Peck discovered a drug that was effective for treating severe acne.
Isotretinoin, a retinoid synthesized by Hoffmann-LaRoche (Nutley, New Jersey) in the 1960s and patented in 1969, was initially intended to be a preventive agent for skin cancer. In the 1970s, Peck, who was a senior investigator in NIH’s Dermatology Branch (then in the National Cancer Institute, NCI; now in the National Institute of Arthritis and Musculoskeletal and Skin Diseases), discovered that isotretinoin was an effective treatment for severe acne.
When Peck started his career in NCI’s Dermatology Branch in July 1969, he learned that the research he had expected to continue—on the isolation and characterization of epidermal keratohyaline granules in newborn rat skin—was being studied in fetal calf hooves by another senior investigator in the Dermatology Branch. Determined to find a different area of study, Peck spent six months reviewing medical literature in the NIH Library and became fascinated by Dame Honor Fell’s (Cambridge University, in Cambridge, England) work on modifying the differentiation pathway of fetal chicken skin in culture by adding retinol to the medium. Instead of becoming keratin-producing, the embryonic chick epidermis became mucin-producing, a process called mucous metaplasia. Peck chose it as his research area and eventually started to study the effect of oral retinoids in treating skin disease. At the same time, then–NCI investigator Michael Sporn (now at Geisel School of Medicine at Dartmouth College in Hanover, New Hampshire) was studying isotretinoin as a possible lung-cancer preventive agent.
It had been known since 1940 that retinoids could be used to treat a variety of skin diseases. Some of the earliest articles were written in the 1940s by NIH investigator Samuel Peck (no relation), who used vitamin A to treat Darier disease, a skin condition characterized by wartlike blemishes on the body (Arch Dermatol Syphilol 43:223–229, 1941). In 1975, Gary Peck contacted Hoffmann-LaRoche about testing isotretinoin in all dermatological diseases that had been treated with oral or topical retinoic acids—acne, psoriasis, and genetic disorders of the skin—and as a preventative for skin cancer.
In 1977, Peck began a four-month, placebo-controlled, double-blind clinical trial that tested isotretinoin in treatment-resistant acne. When some of the patients developed chapped lips, a sign that they were on the medication and not the placebo, the double-blind design was broken at the first four-week follow-up visit. Fortunately, Peck said, there were already significant statistical differences between the drug and placebo in the therapeutic responses at the four-week time point. Most of the patients were either eventually cured of severe acne or had long-term remissions without continuing therapy. (New Engl J Med 300:329–333, 1979).

CREDIT: GARY PECK
Photo of someone’s back covered with cystic acne (left) and later (right) after successful treatment with isotretinoin.
Peck’s study was pivotal to FDA’s approval, in 1982, of Hoffman-LaRoche’s isotretinoin (trade name Accutane) as an oral prescription medication for treating severe acne. Since then, there has been a dramatic drop in the number of cases of severe acne because patients are being treated with isotretinoin at earlier stages of their disease. When the patent expired in 2002, generic versions of isotretinoin were produced and approved by the FDA and are now marketed under many different names by several companies in the United States. Acne is a disease of the sebaceous (oil) glands. Isotretinoin inhibits the production of sebum to shrink these glands. It also inhibits hyperkeratinization (abnormally rapid shedding of skin cells) at the oil glands’ pores and prevents blackheads from forming. Severe birth defects, miscarriage, and stillbirth are among the most serious side effects of isotretinoin, so women of childbearing age are required to use birth control to prevent pregnancy when taking the drug.
Thanks to Peck’s contributions, isotretinoin has been used by millions of people worldwide. The social and psychological benefits of treating potentially scarring, severe acne have been overwhelming. Universally recognized in the field of dermatology, Peck’s many awards include the 2002 Discovery Award of the Dermatology Foundation, the highest award in dermatology.
Gary Peck earned his M.D. from the University of Michigan Medical School (Ann Arbor, Michigan) and completed his dermatology residency training at the University of Chicago Hospitals. After working in NCI’s Dermatology Branch as a senior investigator from 1969 to 1990, he was a professor of dermatology at the University of Maryland Medical School (Baltimore) for three years. In 1994, he joined the Washington Cancer Center Institute, at Washington Hospital Center (Washington, D.C.), where he founded and directed the Melanoma Center. In 2015 he was made director emeritus and is now practicing as a melanoma specialist at the Dermatologic Surgery Center of Washington (Chevy Chase Maryland).
More details can be found in Peck’s full oral history at https://history.nih.gov/display/history/Peck%2C+Gary+2021

E. Gordon Margolin, M.D., a retired internist and nephrologist, has been a volunteer in the Office of NIH History and Stetten Museum since 2011. He interviews NIH scientists for oral histories (including Gary Peck), writes articles on NIH history for The NIH Catalyst, and helps the office in many other ways. Before moving to Bethesda, Maryland, in 2010, he was the director of medicine at Cincinnati Jewish Hospital and a professor of medicine, specializing (in later years) in geriatrics, at the University of Cincinnati. Outside of his volunteer activities, he enjoys playing bridge, reading novels (historical and mystery), and exchanging views with his two adult grandchildren.
This page was last updated on Friday, January 28, 2022
