Research Briefs
CC, NCBI (NLM): NIH CLINICAL CENTER PROVIDES ONE OF THE LARGEST PUBLICLY AVAILABLE CHEST X-RAY DATASETS TO SCIENTIFIC COMMUNITY
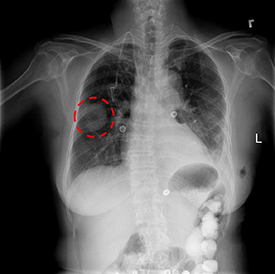
CREDIT: NIH CLINICAL CENTER
A chest x-ray identifies a lung mass.
The NIH Clinical Center recently released over 100,000 anonymized chest X-ray images and their corresponding data to the scientific community. The release will allow researchers across the country and around the world to freely access the datasets and increase their ability to teach computers how to detect and diagnose disease. Ultimately, this artificial intelligence mechanism can lead to clinicians making better diagnostic decisions for patients. The dataset of scans, which was rigorously screened to remove all personally identifiable information, is from more than 30,000 patients, including many with advanced lung disease.
Reading and diagnosing chest X-ray images may seem a relatively simple task for radiologists, but in fact, it is a complex reasoning problem that often requires careful observation and knowledge of anatomical principles, physiology, and pathology. Such factors increase the difficulty of developing a consistent and automated technique for reading chest X-ray images while simultaneously considering all common thoracic diseases.
The hope is that computers will be taught to read and process extremely large numbers of scans, to confirm the results radiologists have found, and to potentially identify other findings that may have been overlooked.
“The international demand for the dataset has been nothing short of astounding,” said Senior Investigator Ronald Summers, who led the initiative. “We are seeing downloads occurring 24 hours a day, seven days a week, already numbering in excess of 1,000 downloads to date.” (NIH authors: X. Wang, Y. Peng, L. Lu, Z. Lu, M. Bagheri, and R.M. Summers, IEEE CVPR 2097–2106, 2017)
NCI: DNA LINKING NUMBER PARADOX SOLVED
Thanks to James Watson and Francis Crick, we know that the shape of DNA is a double helix. Thanks to NIH’s Marshall Nirenberg, we cracked the genetic code. And now, thanks to NCI researchers, we have found the solution to a discrepancy that Crick noticed in 1975: the DNA Linking Number Paradox. Here’s the story.
The DNA double helix is repeatedly supercoiled in the nucleoprotein particles called nucleosomes, which play an essential role in regulating all DNA-dependent processes such as transcription, replication, recombination, and repair. A typical nucleosome contains about 145 base pairs of DNA that make 1.7 left-handed superhelical turns around a histone octamer (an eight-protein complex). The number of times each DNA strand winds around the other is called the linking number (the quantitative measure of DNA topology).
Crick and other scientists discovered a discrepancy between the number of DNA supercoils measured in solution and the number expected from the X-ray crystal structure of the nucleosome core. The crystal structure predicts the generation of 1.7 superhelical turns per nucleosome. But, measurements of DNA topology in circular minichromosomes (small-chromatin-like structures) in viruses or in nucleosome arrays reconstituted from histones and circular DNA showed that there were only 1.0 superhelical turn per nucleosome. This discrepancy is known as the linking number paradox. There have been several untested theories to explain it. The current paradigm is that the difference between the expected and observed numbers of DNA supercoils is related to certain changes in the DNA structure when it folds in nucleosome core. The NCI researchers, however, used topological electrophoretic assays and electron microscopy (EM) to demonstrate that, in fact, the linking number strongly depends on the nucleosome spacing and varies from 1.4 to 0.9. In other words, the DNA supercoiling can change by as much as 50 percent depending on the length of the DNA linker between nucleosomes. Such a strong dependence of DNA supercoiling on the variation in nucleosome spacing generates topological polymorphism of chromatin that can affect the level of transcription.
Future studies, especially detailed 3-D analysis by advanced imaging techniques such as high-resolution cryo-EM tomography, should reveal the actual DNA configurations in active and repressed chromatin and thus perhaps suggest the functional advantages of different chromatin shapes. (NIH authors: T. Nikitina, D. Norouzi, V.B. Zhurkin, Sci Adv 3:e1700957, 2017; Note: the EM was performed by S.A. Grigoryev at Pennsylvania State University College of Medicine, Hershey, Pa.)
NICHD: HEALTHY LIFESTYLE REDUCES HEART ATTACK, STROKE RISK AFTER GESTATIONAL DIABETES
Women who have had gestational diabetes may be able to reduce or even eliminate their elevated risk for cardiovascular disease by following a healthy lifestyle in the years after giving birth, according to a study led by NICHD researcher Cuilin Zhang. The researchers analyzed data from the Nurses’ Health Study, which followed health habits and medical history of more than 90,000 women from before pregnancy through middle age and the early senior years. The study confirms the links between gestational diabetes and cardiovascular disease found by other studies. It also provides some of the strongest evidence to date that cardiovascular disease after gestational diabetes isn’t inevitable for women who adopt a healthy diet, maintain a healthy weight, exercise moderately, and do not smoke. In the current study, the researchers found that women who failed to adopt a healthy lifestyle in the wake of gestational diabetes had a 43 percent higher risk for cardiovascular disease, particularly heart attack and stroke. (NIH author: C. Zhang, JAMA Intern Med DOI:10.1001/jamainternmed.2017.2790)
NIEHS: DNA DAMAGE CAUSED BY CANCER TREATMENT REVERSED BY ZATT PROTEIN
An international team led by scientists at NIEHS is the first to discover a new way that cells fix an important and dangerous type of DNA damage known as a DNA-protein cross-link (DPC). The researchers found that a protein named zinc finger protein 451 (ZATT) can eliminate DPCs with the help of another protein, tyrosyl-DNA phosphodiesterase 2 (TDP2). Because DPCs form when individuals receive some types of cancer treatments, understanding how TDP2 and ZATT work together to repair the damage may improve the health outcomes of cancer patients. Chemotherapeutic drugs can induce DPCs and so can many antibiotics. (NIH authors: M.J. Schellenberg, L.R. Butler, J.G. Williams, G.A. Mueller, R.E. London, and R.S. Williams, Science 357:1412–1416; 2017. DOI:10.1126/science.aam6468.)
NIAID: MULTIPLE RESEARCH APPROACHES ARE KEY TO PANDEMIC PREPAREDNESS
Preparedness in the face of major disease outbreaks can save thousands of lives. Rapid deployment of effective diagnostics, treatments, and vaccines may potentially even stop the disease from exploding into a pandemic. A viewpoint article by NIAID Director Anthony S. Fauci and colleagues examined the multifaceted nature of effective preparedness and the particular role that biomedical research plays. Specifically, the article examined three approaches to pandemic preparedness: pathogen-specific research, platform-based technologies, and prototype-pathogen efforts. Using vaccine development as an example, the authors concluded that a combination of all three approaches will lead to the best preparedness for future pandemics. By investing in research to develop specific countermeasures for known threats and using platform-based and prototype-pathogen approaches to allow for adaptation when unexpected outbreaks arise, global public-health organizations can best prepare to combat future disease outbreaks. (NIAID authors: H.D. Marston, C.I. Paules, and A.S. Fauci, JAMA DOI:10.1001/jama.2017.15033)
NINDS: NIH RESEARCHERS UNCOVER DRAIN PIPES IN OUR BRAINS
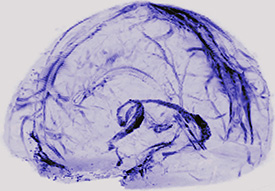
IMAGE CREDIT: D. REICH LAB, NINDS
An MRI scan of a human brain scan showing lymphatic vessels.
By scanning the brains of healthy volunteers, NINDS researchers saw the first, long-sought evidence that our brains may drain some waste out through lymphatic vessels, the body’s sewer system. The results further suggest the vessels could act as a pipeline between the brain and the immune system. To look for the vessels, the team used magnetic-resonance imaging to scan the brains of five healthy volunteers who had been injected with gadobutrol, a magnetic dye typically used to visualize brain blood vessels damaged by diseases, such as multiple sclerosis or cancer. The dye molecules are small enough to leak out of blood vessels in the dura but too big to pass through the blood–brain barrier and enter other parts of the brain. The researchers also found evidence for blood and lymph vessels in the dura of autopsied human brain tissue. Moreover, scans and autopsies of brains from nonhuman primates confirmed the results seen in humans, suggesting the lymphatic system is a common feature of mammalian brains. The team plans to investigate whether the lymphatic system works differently in patients who have multiple sclerosis or other neuroinflammatory disorders. (NINDS authors: M. Absinta, S.-K. Ha, G. Nair, P. Sati, N.J Luciano, M. Palisoc, A. Louveau, K.A Zaghloul, S. Pittaluga, J. Kipnis, and D.S. Reich, eLife 2017;6:e29738; DOI:10.7554/eLife.29738)
NIAID: THREE-IN-ONE ANTIBODY PROTECTS MONKEYS FROM HIV-LIKE VIRUS

CREDIT: SANOFI
Diagram of the “three-in-one” HIV antibody. The blue, purple, and green segments each bind to a different critical site on the virus.
A three-pronged antibody made in the laboratory protected monkeys from infection with two strains of simian human immunodeficiency virus (SHIV) better than the individual natural antibodies from which the engineered antibody is derived, researchers from NIAID and the pharmaceutical company Sanofi (Paris) reported recently. The three-pronged antibody, created by investigators from the National Institutes of Health (NIH) and Sanofi, also stopped a greater number of HIV strains from infecting cells in the laboratory more potently than natural, single antibodies. This new, broadly neutralizing antibody binds to three different critical sites on HIV.
Plans are underway to conduct early-phase clinical trials of the trispecific antibody in healthy people and in people living with HIV in the hope that it could eventually be used for long-acting HIV prevention and treatment. By binding to three different sites on the virus, the new antibody should be harder for HIV to dodge than natural, single antibodies. The ability of trispecific antibodies to bind to three independent targets at once could make them a useful prototype for treatments developed not only for HIV but also for other infectious diseases, autoimmune diseases, and cancers, according to the study authors. (NIAID researchers: A. Pegu, N. Doria-Rose, K. McKee, M. Louder, S.D. Schmidt, Z. Mankoff, Y.D. Kwon, T. Zhou, K. Chen, R.T. Bailer, K. Wang, M. Choe, S. O’Dell, J.-P. Todd, M. Roederer, R.A. Koup, P.D. Kwong, and J.R. Mascola, Science 2017; DOI:10.1126/science.aan8630)
NIEHS: GULF-SPILL OIL DISPERSANTS ASSOCIATED WITH HEALTH SYMPTOMS IN CLEANUP WORKERS

PHOTO CREDIT: JAMES REMINGTON, NIEHS
In May 2010, cleanup workers in Venice, Louisiana, pressure washed oil booms to remove oil, debris, and dispersants.
Workers who were likely exposed to dispersants while cleaning up the 2010 Deepwater Horizon oil spill experienced a range of health symptoms including cough and wheeze, skin irritation, and eye irritation, according to scientists at NIEHS. The study is the first research to examine dispersant-related health symptoms in humans.
Oil dispersants are a blend of chemical compounds used to break down oil slicks into smaller drops of oil, making them easily degraded by natural processes or diluted by large volumes of water. The study estimated the likelihood of exposure to dispersants, based on the types of jobs the workers did and where. Individuals who handled dispersants, worked near where dispersants were being applied, or had contact with dispersant equipment reported the symptoms they experienced during oil-spill cleanup as part of the Gulf Long-term Follow-up (GuLF) STUDY.
After the oil spill, two chemical dispersants, Corexit EC9500A or Corexit EC9527A, were used in some areas where oil was present. Because it was the first time oil dispersants had been used on such a large scale, the researchers said it was important to examine the possible health effects. Most of the previous research on dispersants focused on how well the compounds dispersed oil and the potential environmental impacts. Several small-animal studies that tested the chemicals in dispersants suggested some of the compounds were toxic.
The ongoing GuLF STUDY research is important for shedding light on the potential health impacts associated with an oil spill. GuLF STUDY participants completed telephone interviews during enrollment, a subsequent home visit that included medical assessments and collecting biological samples, and one follow-up telephone interview. A new follow-up interview is scheduled to start fall 2017. The data used in this study came from enrollment interviews with 31,609 English- or Spanish-speaking persons who were involved in oil-spill response or cleanup. (NIEHS authors: C.J. McGowan, R.K. Kwok, L.S. Engel, and D.P. Sandler, Environ Health Perspect DOI:10.1289/EHP1677)
NIMH: LIFE-SAVING POST-ER SUICIDE PREVENTION STRATEGIES ARE COST EFFECTIVE

PHOTO CREDIT: MIKE G/THINKSTOCKPHOTOS.COM
Three interventions designed for follow-up of patients who are identified with suicide risk in hospital emergency departments save lives and are cost effective relative to usual care. A study led by researchers at NIMH modeled the use of the approaches in emergency departments and found that all three interventions compared favorably with a standard benchmark of cost-effectiveness used in evaluating health-care costs. One intervention, sending caring postcards or letters after an emergency-room (ER) visit, is more effective and less expensive than usual care.
According to the Centers for Disease Control and Prevention, suicide is the 10th leading cause of death in the United States; 44,193 people died by suicide in the United States in 2015 (the most recent year for which statistics are available). One approach to reducing the suicide rate is to direct prevention strategies at high-risk groups or settings. An example is emergency departments, which according to the CDC, treat more than 500,000 people each year for self-harm injuries.
Research has found several emergency department–based interventions effective in preventing post-emergency suicide attempts, but none has been widely disseminated or adopted yet. 1) Postcards: Hospital staff mail follow-up postcards each month for four months to all patients identified as at risk, and then every other month for a total of eight cards; 2) Telephone outreach: One to three months after discharge, hospital staff call patients to offer support and encourage engagement in follow-up treatment; 3) Cognitive behavioral therapy: Hospital staff connect patients to a suicide-focused cognitive behavioral therapy program.
Each of these interventions has been tested via randomized controlled trials and found to reduce patients’ suicide risk on the order of 30 to 50 percent. The current study extends this prior research by estimating the cost-effectiveness of these interventions relative to usual care. The authors also point out that even if these prevention approaches were widely used, their impact is limited by the extent to which people at risk are identified for treatment through screening. (NIMH authors: P. Denchev, J.L. Pearson, and M. Schoenbaum, Psychiatr Serv appips201600351, 2017; DOI:10.1176/appi.ps.201600351)
NHGRI: SEQUENCING ALL 24 HUMAN CHROMOSOMES MAY HELP IMPROVE PRENATAL GENETIC SCREENING
Extending noninvasive prenatal screening to all 24 human chromosomes can detect genetic disorders that may explain miscarriage and abnormalities during pregnancy, according to a study by researchers from NHGRI and other institutions. Typical genomic tests performed during pregnancy have targeted extra copies of chromosomes 21, 18, and 13, but they have rarely evaluated all 24 chromosomes. The study findings may ultimately improve the accuracy of these tests, including by explaining why some give false-positive results. The investigators analyzed DNA sequence data from nearly 90,000 samples of maternal plasma and found that pregnancies at greatest risk of serious complications were those with very high levels of abnormal cells in the placenta. The results suggest that patients be given the option of receiving test results from all 24 chromosomes. (NIH author: D.W. Bianchi, Sci Transl Med 9:pii:eaan1240, 2017: eaan1240; DOI:10.1126/scitranslmed.aan1240
NIAID: MECHANISM OF INCREASED CARDIOVASCULAR RISKS WITH HIV
Scientists at NIAID, the Frederick National Laboratory for Cancer Research, and other institutions have expanded the understanding of how chronic inflammation and persistent immune activation associated with human immunodeficiency virus (HIV) infection drive cardiovascular disease risk in people living with HIV. People with HIV are up to twice as likely to experience heart attacks, strokes, and other forms of cardiovascular disease as people who do not have the virus, even when HIV infection is well-controlled by antiretroviral therapy. The scientists found that certain immune cells proliferate in people with HIV, expressing proteins and triggering inflammation and abnormal blood clotting. These processes can be blocked in cells and in nonhuman primate models with the experimental drug Ixolaris. When researchers tested blood samples from people with HIV, they found elevated concentrations of immune cells called monocytes that expressed high quantities of tissue factor (TF), a protein associated with blood clotting and inflammatory processes. The same elevated concentrations of TF-expressing monocytes were observed in monkeys infected with simian immunodeficiency virus (SIV), the monkey form of HIV. The researchers administered Ixolaris to five of them; the Ixolaris-treated monkeys had lower concentrations of biomarkers that predict abnormal blood clotting and immune activation. Although Ixolaris has not been tested for safety or its ability to prevent abnormal clotting in humans, these data suggest that targeting this cellular mechanism may slow the inflammation and clotting processes that place people with HIV at a higher risk of cardiovascular problems. (Frederick National Lab author: M.E. Schechter; NIAID authors: B.B. Andrade, K.W. Tosh, A. Singh, V. Sheikh, D. Ma, A. Sher, I.M.B. Francischetti, and I. Sereti, Sci Transl Med 2017; DOI:10.1126/scitranslmed.aam5441)
This page was last updated on Saturday, January 18, 2025
