Using 3-D Printing to Assess Radiation Exposure
PHOTO BY DANIEL SONE, NCI
Choonsik Lee (right) and Matthew Mille with their coffee-machine size 3-D printer that brews up tools for health physicists to improve their estimates of radiation dose.
Three-dimensional (3-D) printing has been used in medicine since the mid-1990s, primarily in the planning of complicated surgical procedures, then rapidly evolving to include 3-D-printed prosthetic limbs, skin, airway splints, and ears. In the past 10 years, the cost of consumer-grade 3-D printers brought the technology within reach of a far wider audience and research applications including epidemiology.
In a lab at the National Cancer Institute (NCI), a 3-D printer about the size of a coffee maker sits atop a table, periodically whirring away as its heated nozzle extrudes plastic in precise patterns. This printer is brewing up tools for health physicists to improve their estimates of radiation dose for epidemiological studies. Choonsik Lee, senior investigator in NCI’s Radiation Epidemiology Branch (REB) and head of the Dosimetry Unit, and REB postdoctoral fellow Matthew Mille are pioneering these techniques as part of the NCI-Division of Cancer Epidemiology and Genetics (DCEG) dosimetry program.
Modeling Radiation Dose: A Two-pronged Approach
Dosimetry, in the fields of medical physics and radiation protection, refers to the calculation of radiation dose received by the human body. Absorbed dose is a measure of the amount of energy deposited per unit of mass. This estimate is a necessary input for risk assessment for exposed individuals as well as for epidemiological investigations that evaluate the associations between radiation and adverse health effects such as cancer. Medical procedures, ranging from X-ray computed tomography (CT) scans to proton therapy, are a common source of ionizing radiation.
The absorbed dose for specific organs (“organ dose”) depends on many factors, including the depth of the organ in the body, the density of the surrounding tissues, the size of the patient, and the specifics of the procedure. To make sense of this complexity, Lee’s group uses “phantoms,” or models of the human body, that absorb radiation in a similar way to an actual patient. These phantoms can be purely computational, existing as lines of code and images within a computer, or they can be physical mannequins, custom-made of plastic and other materials. Each type has strengths and weaknesses; the investigators need both to accurately assess the radiation dose received by an individual.
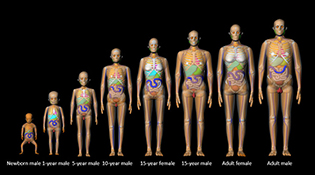
A “family picture” of computational phantoms, modeling a range of ages from newborn to adult.
Physical phantoms are made of stackable layers, each one dotted with a grid of holes in which tiny radiation sensors called dosimeters are inserted. A sensor-packed physical phantom exposed to a radiation source (such as a CT scanner) can provide very reliable dose measurements, but doing so is expensive and time-intensive. Furthermore, the measured doses are constrained by the limited variety of physical phantoms available for purchase.
Computational phantoms used in computer simulations fill in the gaps, accounting for doses to a wider range of body characteristics and machine settings. Because they are virtual, these models are cheaper to test (they don’t require time in the CT scanner), and the calculations can be accelerated using high-performance computing clusters. The computer models still depend, however, on some measurements from physical phantoms to provide realistic benchmark measurements and validation.
Customization of the Phantoms
Mille became interested in the possibility of using 3-D printing to build phantoms early in his graduate studies. The project gained momentum once he found an enthusiastic mentor in Lee. Although life-size physical phantoms are available for purchase from a few manufacturers, they are very expensive and their relatively simple designs have not changed for decades.
“Our goal is to use 3-D-printing technology to customize phantoms and make them more realistic and versatile,” said Mille. “For instance, the two physical models the [DCEG] has now are both male. To simulate exposure to breast tissue, we can print prostheses to be attached to the male phantom to estimate radiation doses from breast-cancer treatment.” In addition to reducing costs, the researchers hope to create physical phantoms that more closely resemble their sophisticated computational models and are more anatomically accurate and customizable.
Lee is also experimenting with how to incorporate patient body size into dose estimates. “There are no obese physical phantoms,” he said. A recent study he led, published in the American Journal of Roentgenology, showed that using a normal-weight reference phantom to assess dose to an obese patient using particular CT machine settings can lead to overestimating the organ dose by as much as 200 percent (AJR Am J Roentgenol 208:1082–1088, 2017). The team developed an ingenious solution: Printing layers of “body fat” that can be attached to an existing phantom.
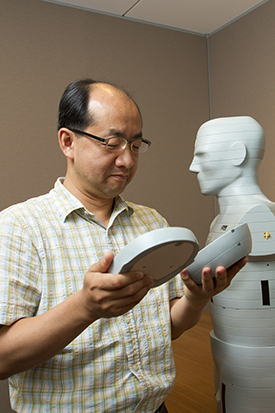
PHOTO BY DANIEL SONE, NCI
Lee examines layers of one of his commercially produced phantoms. Physical phantoms are composed of stacked layers into which radiation sensors are inserted for testing. Inset: Different colors in the layer approximate various body tissues such as bone or muscle. Small holes for sensors dot the slice; when not in use, the holes are filled with plugs.

“The presence of extra body fat effectively shields organs from external sources of radiation,” said Mille. “Consequently, technical parameters in CT imaging must be altered for obese patients to maintain good image quality. This [alteration] can result in higher doses for obese patients compared [with] those with a normal [body mass index].”
As part of this work, the team is exploring how 3-D printing materials can be used to mimic the radiation attenuation characteristics of human tissues with different mass density, such as fat, soft tissue, lung, and bone. To ensure that the printed phantom parts appropriately simulate human tissue, Mille images them on a CT scanner and compares the resulting images with those taken of real patients. Through this work, the researchers hope to create physical phantoms that respond to radiation in the same way as a patient.
Adapting to New Technologies
Innovation in the use of radiation in medical practice requires invention on the part of dosimetrists as well. For example, existing physical phantoms are inadequate for evaluating exposure to secondary neutrons produced inside the body during proton therapy, an emerging type of cancer treatment. Gleb Kuzmin, a predoctoral fellow in REB who also works with Lee, is spearheading research to estimate organ doses from such treatments. Step one addresses a simple, yet stubborn, problem: The holes in each layer of the commercial phantoms are too small to fit a neutron detector. The obvious solution—drilling larger holes—is not an option, because modifying the expensive phantom for this test would make it less effective with the smaller dosimeters. Instead, the team will print copies of select slices of the human body with larger openings to accommodate the neutron detectors. Once the patchwork phantom is put back together, Kuzmin can validate his simulations by testing it in a proton treatment system and measuring the absorbed dose.
Emphasis on Collaboration
“These phantoms have truly been an ‘NIH family’ effort,” said Lee. Many individuals have contributed their time and ideas, including Jacob Oshinsky, a 12-year-old 3-D-printing whiz and son of DCEG staff scientist Stephanie Weinstein. On Take Your Child to Work Day in 2016, Jacob visited the 3-D-printing lab and introduced the dosimetry team to a range of different printing materials.
Through a collaboration with Roberto Mass-Moreno, of the Radiology and Imaging Sciences Department at the NIH Clinical Center, REB investigators have access to the center’s state-of-the-art imaging equipment with which they can test the printed phantoms.
The partnerships extend to the National Institute of Standards and Technology (NIST) in Gaithersburg, Maryland, where some initial CT scanning was performed. Staff at the NIST Research Reactor are also helping to test novel printing materials. They expose the materials to a low-energy neutron beam emanating from the reactor to determine their elemental composition and, by extension, their radiation-absorption properties.
“DCEG has always been at the forefront of efforts to increase the public-health impact of epidemiology by improving tools and methods,” said REB chief Amy Berrington de González. “The 3-D-printed dosimetry phantom project by Drs. Lee and Mille is a perfect example of this cutting-edge work.”
Working together, these scientists aim to build more realistic human phantoms that will help to improve our understanding of the risks of medical radiation. There remain many challenges to overcome, but the researchers are optimistic. “Our research so far has found that, with some resourcefulness, much can be accomplished despite limitations of current 3-D printing technology,” said Mille. “It is only a matter of time until a life-size human phantom can be printed with the push of a button. We think we’ll clone Dr. Lee first!”
From NCI-DCEG Research News and Highlights: http://bit.ly/2uemrs1
This page was last updated on Monday, April 11, 2022
