Tracking Sickle Cell Symptoms With Infrared Light
New IRP Study Supports Non-Invasive Way to Gauge Blood Vessel Health
IRP research suggests light-based technologies may one day supplement or replace blood tests for people with sickle cell disease.
Nobody likes being jabbed with a needle for blood tests, but for people with sickle cell disease, it’s a necessary and frequent annoyance to make sure their condition is under control. However, blood tests may become less needed in the future for those patients thanks to new IRP research that has identified ways to measure certain health metrics using non-invasive, light-based technologies.1
In most people, red blood cells are round discs resembling wheels or inner tubes, but in people with sickle cell disease, they have a deformed, sickle-like shape that makes them prone to getting stuck in blood vessels. This can cut off the oxygen supply to organs, placing patients at risk for strokes and organ damage, and it also triggers excruciating episodes called sickle cell ‘crises.’ Right now, the only way to tell how many of those misshapen blood cells are flowing through a patient’s body — and therefore their risk for a related health incident — is with a blood test.
“Typically, when you’re doing conventional tests, they’re going to be something that needs to be done at a hospital or a medical provider’s office, and it’s going to take time, it takes resources, and it takes a trained technician to draw blood and run tests on it,” explains IRP staff scientist Timothy Quang, Ph.D., the study’s lead author. “It’s not trivial to do these tests, and even though sickle cell patients have these recurring, unpredictable pain crises, doing these kinds of tests on a frequent basis is just not feasible.”
Dr. Quang and his colleagues in the lab of Bruce Tromberg, Ph.D., Director of NIH’s National Institute of Biomedical Imaging and Bioengineering (NIBIB), are working on alternatives to those tests. They are specifically studying ‘optical’ techniques that use certain wavelengths of light to glean information about the makeup of tissue.
“If I were to put a flashlight up against my finger right now, you’d see that all the red light comes through my finger,” Dr. Quang says. “That gives us an indication that red light can go deeper into tissue without getting absorbed by everything. We use technologies that use light in that red or near-infrared range because that light penetrates deeply into tissue, and that means we can look at the brain, blood, and muscle non-invasively. Based on how the light is absorbed, we can recover information about the concentration of different biomolecules.”

Optical imaging setup for the sickle cell disease study. The bounding box (right) features a closer view of the optical probes that capture information about the blood in the fingertip (A), skin (B), and muscle (C).
In the new study, Dr. Quang and his IRP colleagues took measurements using two such optical technologies and compared them to the metrics provided by traditional blood tests. Their study piggy-backed on a clinical trial being conducted at NIH, which aimed to test whether a chemical called isoquercetin could combat the blood vessel inflammation seen in people with sickle cell disease.
Although isoquercetin did not seem to have any noticeable effect on the patients enrolled in the study, the optical measurement techniques proved promising. During the patients’ ‘baseline’ assessment, before they started the treatment, those who had a higher concentration of red blood cells in their blood — a blood test measurement known as ‘hematocrit’ — also tended to have higher concentrations of oxygen in their blood as measured by the optical techniques. Higher hematocrit was also associated with lower values in a factor measured with optical techniques in the study called ‘oxygen extraction fraction,’ which calculates the percentage of oxygen that cells in an area of the body are extracting from the blood.
In addition, patients whose blood was more prone to changing from a normal liquid to a potentially problematic semi-solid form — a process known as ‘coagulation’ — produced lower values on an optical measurement that gauges how quickly blood returns to an area of the body when the blood flow has been cut off by a fully-inflated blood pressure cuff. That same optical measurement also tended to be lower in people with higher levels of a marker of inflammation called intracellular adhesion molecule 1 (ICAM-1), which is measured via blood test.
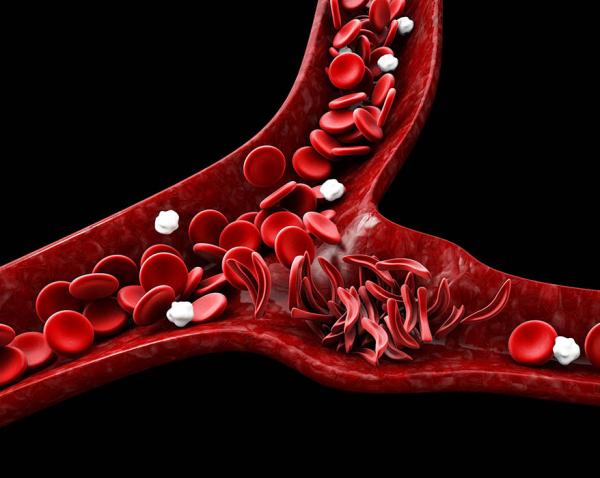
The sickle-shaped red blood cells of sickle cell patients can get stuck in blood vessels. The more of those abnormal cells a patient has, the more inflamed their blood vessels become and the higher their risk for health complications.
“For sickle cell disease patients, because their red blood cells are much more fragile, you have a lot of cell fragments bouncing around blood vessels, and those can damage the walls of the vessel and make them inflamed, which makes the vessel narrower and less reactive,” Dr. Quang explains. “That inflammation limits how quickly blood can return to a part of their body, so we can use this test to figure out how pliable their blood vessels are.”
What’s more, those relationships between the blood test measurements and the optical measurements were consistent over the course of the entire study. In other words, if a blood test value tended to increase or decrease over during the study for a particular patient, the optical measurement related to it during the baseline assessment usually changed in the expected way over the course of the study for that individual.
“If we’re able to see this one relationship on one day in this group of patients, then in theory, if we look at those same patients a month from now, we should be able to see the same relationship,” Dr. Quang says. “That gives us confidence that what we’re seeing is a real relationship between these two markers and not just a fluke that we saw on a single measurement day.”
Dr. Timothy Quang (left), the study’s first author, and Dr. Bruce Tromberg (right), its senior author
With more research to verify and expand on the IRP study’s findings, it could one day be possible to gauge the health of people with sickle cell disease using non-invasive optical technologies, sparing them the nuisance of frequent needle sticks to draw blood. What’s more, many scientists are trying to shrink down such technologies so they can be worn by patients constantly as they go about their lives, providing real-time readouts of their health. This would not only reduce how frequently patients need to visit their doctors or a clinic that draws blood for medical tests, but could also provide researchers with information about changes in the body that happen in the run-up to a painful sickle cell crisis.
“If we can take these kinds of technologies and figure out what information can be used to predict when a pain crisis is about to show up, that would be really helpful because right now it’s basically at the drop of a hat — those pain crises can happen at any time,” Dr. Quang says. “If we have something patients can have with them all the time and gives them some early indication that they’re trending in the wrong direction, they can take preventative steps early on.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Quang T, Mostashari G, Berning E, Gopalan BP, Lizarralde-Iragorri MA, Lovins D, Shet AS, Tromberg BJ. Non-invasive optical and laboratory hematologic biomarkers correlate in patients with sickle cell disease. Biomed Opt Express. 2024 Jul 26;15(8):4829-4841. doi: 10.1364/BOE.527770.
Related Blog Posts
This page was last updated on Tuesday, January 7, 2025
