Targeting Tuberculosis
IRP’s Clifton Barry Seeks Novel Therapies for an Ancient Foe
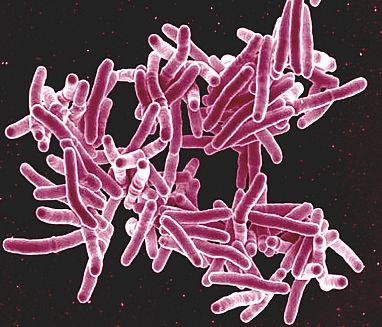
The bacteria that cause tuberculosis are constantly outflanking our best treatments, forcing scientists like the IRP’s Clifton Barry to continuously pursue new ones.
March 24 is World Tuberculosis Day, a day to remember that a preventable and curable disease still kills more than a million people each year. Despite every effort to eradicate it, the disease-causing bug, Mycobacterium tuberculosis, keeps coming back stronger and more ready for a fight. As varieties of the bacteria grow more and more resistant to treatment, an evolutionary war is raging between the bacterium and researchers like IRP senior investigator Clifton Barry, Ph.D., who has been seeking solutions for the past 33 years.
“For most cases of tuberculosis, a first-line course of therapy for six months consists of about $15 worth of pills,” Dr. Barry says. However, if the particular bacteria causing someone’s infection is resistant to those drugs, the costs can rise precipitously, while the chances of a cure plummet. Globally, about 3.6 precent of new cases are drug-resistant, but that jumps to 20 percent in people who have already been treated once. In the resource-poor parts of the world where most tuberculosis cases occur, it’s not uncommon to experience repeated infections throughout life, yet even the $15 cost of the basic treatment is unaffordable for many — not to mention the difficulty of getting the drugs to where they’re needed most.
As a result, researchers must continuously search for new treatments as the bacteria continue outsmarting our available drugs. Unfortunately, the high costs necessary for research and development, especially for large, international clinical trials, aren’t offset by the minimal proceeds new tuberculosis drugs might bring in, so there’s little commercial incentive for large pharmaceutical companies to invest. Instead, that work falls to non-profit research institutions like Dr. Barry’s twin labs at NIH and the University of Cape Town in South Africa, which work with international organizations such as the Gates Foundation’s Tuberculosis Drug Accelerator and the Global Alliance for Tuberculosis Drug Development to scour the world for treatments.
Indeed, Dr. Barry started his NIH career sifting through more than 60,000 different molecules to find ones that might be useful for fighting tuberculosis. One of them, called PA-824, proved effective in killing multi-drug-resistant tuberculosis.1 The road to treating patients, however, was long. Even though Dr. Barry was part of the team that identified PA-824, now called pretomanid, in 2000, it didn’t receive approval from the U.S. Food and Drug Administration (FDA) until 2019. For now, it has become a go-to treatment for many forms of multi-drug-resistant tuberculosis, but it’s not a panacea.

Dr. Clifton Barry
In another case, about 20 years ago, Dr. Barry and his colleagues took a new approach to an existing antibiotic and found success. Linezolid, a wide-spectrum antibiotic, is commonly used to knock out a variety of different infections quickly. However, tuberculosis treatment takes a long time — usually about six months— and linezolid has serious and debilitating side effects when taken for extended periods. Consequently, Dr. Barry’s team partnered with doctors in South Korea to see what would happen if they treated tuberculosis patients with a lower-than-usual dose of Linezolid.
“We were working with doctors at a tuberculosis hospital in South Korea and they were seeing an enormous number of patients come in with extremely drug-resistant tuberculosis, which is basically a death sentence; it was associated with an 80 to 90 percent mortality rate because there were effectively no treatments available to them,” Dr. Barry remembers.
In a randomized, controlled trial with 40 patients, a lower dose of Linezolid administered over several months cured 38 patients without causing serious side effects.2
“The results were stunning enough that the World Health Organization moved linezolid from a drug with no known use against tuberculosis to an essential medicine for drug-resistant tuberculosis,” Dr. Barry says. “I think it’s had a huge impact on global policy. The global survival rate for patients with extremely drug-resistant tuberculosis has gone way up and I think that’s largely attributable to widespread use of Linezolid.”
While successes like this have made a huge difference in treating drug-resistant strains of tuberculosis, the ancient bacterium has proved nimble in overcoming new attacks, forcing scientists to look for still more options. Dr. Barry and his team recently tried a new idea that stemmed from a very old source: sphagnum peat bogs.
“We stepped back and asked, ‘How did Mother Nature solve this problem?’” Dr. Barry says. “It’s a really ancient bacterium that’s been with us for as long as humans have been on the planet.”
He recalled that epidemiological studies conducted in the 18th century identified high numbers of leprosy cases among people who lived close to peat bogs in Scandinavia, so Dr. Barry asked whether other disease-causing bacteria might thrive in that environment.
“The conditions inside a sphagnum peat bog are actually pretty similar to the conditions inside the human lung,” Dr. Barry explains, because the bog’s mossy top layer — made up of thousands of years’ worth of decaying organic matter — is an acidic and oxygen-poor environment that’s perfect for anaerobic bacteria to grow. Consequently, Dr. Barry and his team visited bogs around the East Coast and collected samples of decayed plant matter from them to search for microbes that might compete for nutrients with the tuberculosis bacteria. They found promising candidates in several types of fungi, which could kill off tuberculosis bacteria when grown alongside them in the lab.

Dr. Barry’s team has found peat bogs to be a surprisingly rich source of microbes that might provide new treatments for tuberculosis.
“These experiments have been remarkably productive,” Dr. Barry says. “In addition to finding another chemical tool to treat tuberculosis, we found a previously overlooked and uniquely vulnerable way to possibly eradicate tuberculosis from people's lungs very quickly.”
While the battle against tuberculosis is far from over, Dr. Barry’s dedication and innovative thinking are paving the way for faster, more effective treatments. He credits NIH’s investment in research and partnership with international organizations for bringing these treatments to market at a rapid clip.
“Over the past five years, we’ve turned into a well-oiled machine,” he says. “We’re producing a new drug candidate every year right now. I think we have made some pretty big progress on the drug discovery side.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Manjunatha UH, Boshoff H, Dowd CS, Zhang L, Albert TJ, Norton JE, Daniels L, Dick T, Pang SS, Barry CE 3rd. Identification of a nitroimidazo-oxazine-specific protein involved in PA-824 resistance in Mycobacterium tuberculosis. Proc Natl Acad Sci U S A. 2006 Jan 10;103(2):431-6. doi: 10.1073/pnas.0508392103. Epub 2005 Dec 30.
[2] Lee M, Lee J, Carroll MW, Choi H, Min S, Song T, Via LE, Goldfeder LC, Kang E, Jin B, Park H, Kwak H, Kim H, Jeon HS, Jeong I, Joh JS, Chen RY, Olivier KN, Shaw PA, Follmann D, Song SD, Lee JK, Lee D, Kim CT, Dartois V, Park SK, Cho SN, Barry CE 3rd. Linezolid for treatment of chronic extensively drug-resistant tuberculosis. N Engl J Med. 2012 Oct 18;367(16):1508-18. doi: 10.1056/NEJMoa12019.
[3] Malhotra N, Oh S, Finin P, Medrano J, Andrews J, Goodwin M, Markowitz TE, Lack J, Boshoff HIM, Barry CE. Environmental sphagnum-associated fungi target thiol homeostasis to compete with Mycobacterium tuberculosis. bioRxiv [Preprint]. 2024 Sep 23:2024.09.23.614403. doi: 10.1101/2024.09.23.614403. Update in: PLoS Biol. 2024 Dec 3;22(12):e3002852. doi: 10.1371/journal.pbio.3002852.
Related Blog Posts
This page was last updated on Monday, March 24, 2025
