Experimental Antibody Tightens Up Leaky Blood Vessels
Treatment Could Benefit Patients With a Variety of Illnesses

Recent IRP research demonstrated that an experimental monoclonal antibody helped stop blood vessels from leaking, a life-threatening problem seen in numerous conditions.
Our blood is a miraculous mix of cells and critical fluids that keep our organs running and fight off dangerous infections. Of course, for blood to do its job, it has to stay in our veins and arteries, which is easier said than done for people with certain illnesses. Fortunately, a recent IRP study has demonstrated the promise of a potential new treatment for people with dangerously leaky blood vessels.1
Several life-threatening conditions, including Ebola and sepsis due to an uncontrolled infection, cause the fluid component of blood to leak out of blood vessels. IRP senior investigator Kirk Druey, M.D., however, came to study the phenomenon through a very rare ailment called Clarkson disease, which causes patients to periodically experience ‘flares’ or ‘episodes’ when their veins and arteries suddenly and inexplicably start leaking.
“Their blood becomes thick with cells and proteins without much fluid, so it becomes kind of like syrup,” Dr. Druey explains. “They can lose as much as 70 percent of their blood volume into their tissues, and they can’t get enough oxygen to their major organs, so they start to shut down.”
Since Dr. Druey is one of the only scientists around the world studying Clarkson disease, it’s not surprising that he was the go-to guy when South Korean pharmaceutical company PharmAbcine wanted someone to gauge the effects of a treatment it had developed for the illness. The drug, a ‘monoclonal antibody’ called 4E2, works by activating a cellular receptor called Tie2 that is found almost exclusively on the cells that line the body’s inner surfaces, including veins and arteries. Activating Tie2 helps those cells, known as endothelial cells, stick together to form a barrier that seals up blood vessels. What’s more, problems with it have been implicated in some diseases that cause leaky blood vessels, although it has not been specifically linked to Clarkson disease.
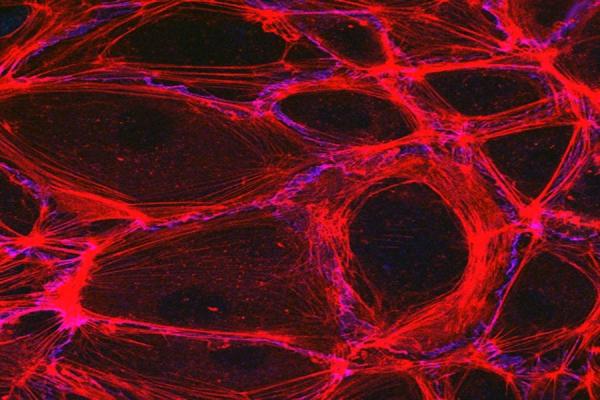
Close-up view of the endothelium, the layer of cells that lines the inside of blood vessels. Actin filaments, shown in red, and cadherin, shown in purple, help endothelial cells stick together and form a tight seal. Image credit: Christoper V. Carman and Roberta Martinelli, Harvard Medical School
Nevertheless, in the new study, Dr. Druey’s team set out to examine whether activating Tie2 using the 4E2 antibody might have beneficial effects for patients with Clarkson disease. The IRP scientists began by isolating cells called blood outgrowth endothelial cells (BOECs) from the blood of healthy people and patients with Clarkson disease. These cells develop from precursors of endothelial cells in the blood, and it is much easier to extract them from blood than it is to get fully mature endothelial cells by scraping the insides of people’s blood vessels with a tiny metal catheter.
“We grow these endothelial cells in petri dishes, and they’re very good at forming a barrier,” Dr. Druey says. “They come into contact with one another and look kind of like a cobblestone street. They’re very tightly bound to each other and they don’t allow leakage of much fluid or protein between them. If you apply an electrical current through the cells, you can get an indirect measure of the electrical resistance that’s being exerted by this layer of cells. Then, when we treat the cells with something that causes vascular leakiness, the cells will come apart from one another and allow more current to pass through them, and so the resistance goes down.”
When Dr. Druey’s team treated those BOECs with the 4E2 antibody, the cells’ electrical resistance increased, signifying that they were forming a tighter barrier than untreated cells. Notably, this effect was nearly twice as large in BOECs from Clarkson disease patients than in cells from healthy individuals.
Dr. Kirk Druey (right), the study’s senior author, with Arturo Porzecanski, who has Clarkson disease.
Next, the researchers exposed the isolated BOECs to various chemicals naturally produced in the body that encourage blood vessels to leak. When they pre-treated the cells with the 4E2 antibody before exposing them to those substances, the cells showed signs that they held together more tightly than cells that were not exposed to the 4E2 antibody.
The IRP team also tested the drug in a mouse model of Clarkson disease that has blood vessels highly prone to leaking when the animal is treated with those same natural chemicals. Just like the isolated BOECs, the mice pre-treated with the 4E2 antibody experienced less vascular leakage than untreated mice when exposed to those substances. As a result, the mice treated with 4E2 were much more likely to survive.
Finally, because respiratory infections like the flu and COVID-19 commonly cause severe vascular leaks in people with Clarkson disease, the researchers infected those same mice prone to vascular leakage with a flu virus and then gave some of them the 4E2 antibody. The animals treated with 4E2 lost significantly less weight due to their illness than the untreated mice and their blood vessels leaked much less.
“That suggests that even in patients who have had flu-like symptoms or a cold for several days, if they took this drug, it might lessen the severity of their episode,” Dr. Druey says.
Treatments for Clarkson disease may also be useful for other conditions that degrade blood vessels, including diabetes, Ebola, and sepsis, in which the body has an out-of-control reaction to an infection.
Overall, the study’s results demonstrate the promising potential of the 4E2 antibody as a treatment for not only Clarkson disease, but also other illnesses that degrade blood vessels — from the acutely life-threatening Ebola virus to more common, chronic conditions like cancer and diabetes. Although it is challenging to organize a clinical trial testing a treatment for a very rare illness like Clarkson disease, Dr. Druey believes it’s well worth the effort to assess 4E2’s effects in people with the condition.
“I think there’s enough evidence from other Tie2-targeting therapies that this would be an effective target,” he says. “I’m not sure if this antibody has gone through phase 1 safety trials yet, but I think other Tie2-targeting antibodies have been used in patients and have been shown to be safe, so it would be worth trying it in patients. There are some logistical barriers to testing new therapies in this disease due to its rarity, but where there’s a will, there’s a way.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
References:
[1] Ablooglu AJ, Desai A, Yoo JS, Park CH, Lee EA, Kim BY, Park H, Lee YA, Shim SR, Lee WS, Druey KM. A ligand-independent Tie2-activating antibody reduces vascular leakage in models of Clarkson disease. Sci Adv. 2023 Nov 15;9(46):eadi1394. doi: 10.1126/sciadv.adi1394.
Related Blog Posts
This page was last updated on Tuesday, March 26, 2024
