A New Approach to Fighting the Flu
Six Questions With Dr. Matthew Memoli
Research by IRP investigator Matthew Memoli could lead to a more effective flu vaccine.
We all know flu season as the time of year where people are loading up on hand sanitizer and heading to the doctor for their flu shot. However, many underestimate the severity of the flu. During a typical flu season, five to twenty percent of Americans fall ill, leading to more than 200,000 hospitalizations and 36,000 deaths. Because of this serious threat to the public, the IRP has a long track record of researching vaccines, antivirals, diagnostics, and other resources in an effort to prevent individuals from catching the flu and improve care for those who do.
Since the 1970s, scientists have evaluated the likely effectiveness of flu vaccines by examining their ability to cause patients’ immune systems to produce protective molecules called anti-hemagglutinin (HA) antibodies. However, the usefulness of this approach had not been re-examined since it was first introduced more than four decades ago.
A 2016 study by Matthew Memoli, M.D., M.S., challenged that previous standard. As the Director of the Clinical Studies Unit in the IRP’s Laboratory of Infectious Disease, Dr. Memoli spear-headed the first study in the U.S. in over a decade that exposed healthy volunteers to the flu virus and examined how their immune systems responded. His study showed for the first time that a different type of molecule produced by the immune system, called anti-neuraminidase (NA) antibodies, are a better predictor of flu protection and more effectively prevented the disease than anti-HA antibodies, the previous ‘gold standard.’
In recognition of National Immunization Awareness Month this month, I spoke with Dr. Memoli to discuss his research on flu protection, his hopes for a universal vaccine, and how his research continues to evolve today.
What prompted you to conduct this study of the flu?
“Before this study, I had been studying influenza in people for a number of years and realized that the types of vaccines we were providing had limitations. For example, vaccines protected some people, but not all. Some people would get the vaccine and still contract the flu, particularly people who really needed protection such as the elderly, small children, and individuals with chronic diseases. The scientific community was working towards a universal vaccine that would protect against all forms of the flu virus, but I am interested in finding a way to make a vaccine universal in the sense that it protects everybody who receives it.
“Looking further into how flu vaccines were developed, I realized that the sole focus of the flu vaccine was creating anti-HA antibodies that protect us from the flu by binding to the hemagglutinin protein found on the virus. When looking at the data that supports this approach, protection is shown to exist, but it isn’t perfect. In fact, most studies show as little as 50 to 60 percent protection.

Dr. Matthew Memoli
“From there, I began to think about other types of immunity that might be important to include in new vaccines because they could cause the vaccine to be more effective in a wider variety of people. I had done a bit of reading and found that, historically, there had been studies that demonstrated that antibodies against the flu protein neuraminidase might be important when it comes to the immune system’s response to flu. However, over the years, the focus had shifted away from neuraminidase and instead turned to hemagluttinin.
"From this research, we designed our study to evaluate two things. First, twe aimed to define what protection the anti-HA antibodies give individuals against the flu virus. Second, we wanted to look for other protective agents, such as antibodies against neuraminidase, and determine their role in protecting against flu.”
What was the most challenging or surprising aspect of this study?
“I wasn’t fully expecting to see the results we gathered. I thought that anti-NA antibodies were important but didn’t realize they were as important as they turned out to be. Initially, I thought that the anti-NA antibodies, in combination with other anti-HA antibodies, would be a predictor of disease. However, we found that the anti-NA antibodies were in fact the only antibodies that were an independent predictor of disease.”
What impact has this research had to date as it relates to flu vaccines?
“I think that this study brought the idea of anti-NA antibodies being protective back into the vocabulary of scientists working on influenza vaccines. Prior to this publication, no one was really investigating, thinking about, or publishing anything related to the protective nature of anti-NA antibodies. However, after the study was published, interest began to spike again.
“For example, after our study, at least two natural infection studies looked at the protective nature of anti-NA antibodies and confirmed our findings that people with more anti-NA antibodies are generally more protected from the flu virus. This approach is being studied further as groups of scientists, including myself, have begun thinking about putting neuraminidase into vaccines in order to produce anti-NA antibodies.
“As the topic continues to be studied, I think that over the next couple of years we’re going to see universal vaccine candidates that use this as part of their overall strategy, if not their sole strategy. In fact, I know that is going to happen because two vaccines are already using this strategy, but I think there will be more.”
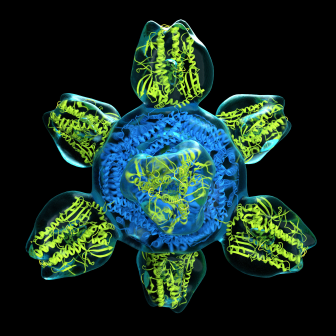
Colorized structure of a prototype for a universal flu vaccine.
What collaborations were important in conducting this research?
“We had been collaborating with one of the few people thinking about neuraminidase at the time, Dr. Maryna Eichelberger. Dr. Eichelberger, who was running a lab at the FDA, had been studying neuraminidase activity and had published assays that measure anti-neuraminidase antibodies.
“Initially, our collaboration in this study consisted of Dr. Eichelberger measuring the antibodies in some of our patients. As the collaboration evolved, she then taught us the technique so that we could measure the antibodies ourselves.
“This was an extremely important collaboration. We would not have been able to reach the results we did without the help of Dr. Eichelberger.”
What failures or issues did you face along the way?
“One of the most memorable obstacles was that around the time we were conducting this study, the Ebola outbreak happened. As a result, a couple of patients were brought to the NIH for treatment. They were brought to the unit that we typically used for this study and took priority, as they should have. This was a minor hiccup as it caused us to unexpectedly rearrange how we were going to accommodate our study.”
How have you continued to study anti-neuraminidase antibodies, and what are your plans to study the topic in the future?
“After completing this study, we used the samples from participants to conduct a follow-up laboratory study. During the follow-up study we measured the anti-HA stalk antibody response, a major focus of current vaccines, to determine how its levels correlated with flu protection compared to anti-NA antibodies. We found that anti-NA antibodies are still the best independent indicator of protection.
“On top of that, at the moment, I am personally developing a neuraminidase-based vaccine, which I am hoping will be used as an independent vaccine or as an adjunct to current vaccines. I hope to have this particular vaccine enter Phase I clinical trials in early 2020. I am really hoping to improve not only the protection vaccines offer, but the breadth of protection.”
Head over to our Accomplishments page for more information on Dr. Memoli’s research, and subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
Related Blog Posts
This page was last updated on Tuesday, May 23, 2023
