Test May Identify Poor Prognosis for Some Patients with Lung Cancer
A panel of three genetic markers may help to identify patients with early-stage lung cancer who have a very strong likelihood of their disease returning after surgery, according to findings from a study by NCI researchers.
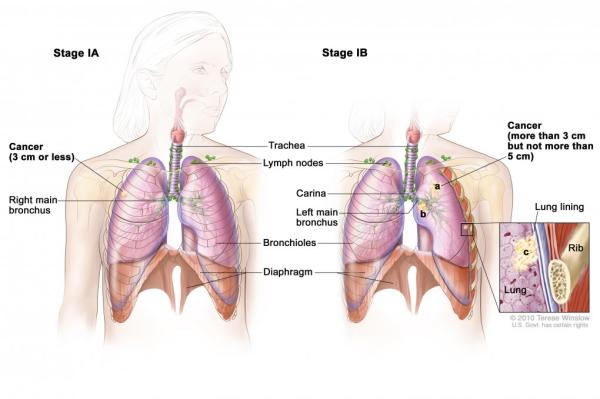
In the retrospective study, patients with stage I lung cancer (adenocarcinoma) whose tumors expressed all three markers were far more likely to die from their cancer or to have a recurrence than patients whose tumors did not express these markers.
Credit: Terese Winslow
A panel of genetic markers may identify patients with stage I lung cancer with a poor prognosis, suggesting that they may benefit from post-surgical chemotherapy.
Post-surgical, or adjuvant, chemotherapy is not currently recommended for most patients with stage I lung cancer because it has not been shown to improve survival. But the three-marker panel, the study authors suggested, may point to a subset of high-risk patients who would be most likely to benefit from it.
The findings were published June 24 in the Journal of Thoracic Oncology.
In patients with stage I disease, tumors are present only in the lungs and can often be removed surgically. Nevertheless, in up to 30 percent of patients, the cancer returns after surgery and they die from the disease within 5 years.
Currently, there is no proven way to identify which of these patients are at increased risk of their disease returning, said the study’s senior author, Curt Harris, M.D., of NCI’s Center for Cancer Research (CCR). This study is the latest in a series from Dr. Harris’ lab investigating whether different biomarkers they have identified might be able to fill this void.
The studies, he explained, are “part of a precision medicine effort to integrate various ‘omics’ into a single platform and develop a classifier for diagnosis and prognosis in patients with stage I lung cancer.”
For this most recent study, the researchers first analyzed tumor and nearby lung tissue samples from patients with stage I lung adenocarcinoma who had been treated at Baltimore area hospitals and at centers in Norway and Japan.
They identified a specific epigenetic change in the HOXA9 gene—that is, a chemical change to the DNA, but not an alteration of the DNA sequence—called hypermethylation that was strongly associated with dying from lung cancer in the ensuing 5 years.
The researchers confirmed the association between HOXA9 methylation status and outcome in two additional cohorts of patients with stage I lung cancer from Japan and the United States and Europe, respectively. Only data on recurrence-free survival were available for these additional cohorts, but patients with stage I disease whose cancers return are at extremely high risk of dying of the disease within 1 year of recurrence, noted the study’s lead author, Ana Robles, Ph.D., also of CCR.
In their earlier studies, Dr. Harris’ team had identified two other genetic markers—overexpression of microRNA-21 and the expression of four genes (XPO1, BRCA1, HIF1alpha, and DLC1)—that also independently correlated with poor 5-year survival in patients with stage I lung cancer.
So, Dr. Robles explained, they combined all three markers into a single classifier and analyzed its association with outcomes in the Japanese and the NCI/Norway cohorts. The classifier “produces a simple score,” she continued, based on how many markers a tumor sample expresses.
The higher the score, they found, the greater the risk of lung cancer death or recurrence.
In the combined NCI/Norway cohort, for example, patients who had not received any post-surgical chemotherapy and whose tumors were positive for one, two, or all three markers had a 2-, 5-, and 43-fold greater risk of lung cancer death within 5 years, respectively.
An accurate prognostic test for patients with stage I disease would have important clinical implications, Dr. Robles said. Based on the Centers for Medicare and Medicaid Services’ recent decision to cover lung cancer screening with low-dose computed tomography (CT) for patients at high risk, its use is already growing. As a consequence, she explained, “many more stage I cancers are going to be diagnosed.”
Dr. Harris’ lab is developing an assay that incorporates all three markers that can be used in prospective validation studies, he explained. They have also begun discussions with diagnostics companies to further develop the test for potential clinical use.
Related Resources
Related Blog Posts
This page was last updated on Tuesday, May 23, 2023
