Smoldering Spots in the Brains May Signal Severe MS
NIH Study Provides Hope for Diagnosing and Testing the Effectiveness of New Treatments for More Disabling Forms of Multiple Sclerosis
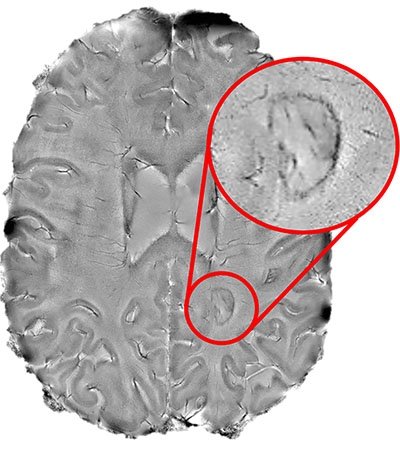
CREDIT: DANIEL REICH LAB, NINDS
NIH researchers found that the dark-rimmed spots, representing ongoing, “smoldering” inflammation, may be a hallmark of more disabling forms of multiple sclerosis.
Aided by a high-powered brain scanner and a 3-D printer, NIH researchers peered inside the brains of hundreds of multiple sclerosis (MS) patients and found that dark-rimmed spots that represent ongoing, “smoldering” inflammation, called chronic active lesions, may be a hallmark of more aggressive and disabling forms of the disease.
“We found that it is possible to use brain scans to detect which patients are highly susceptible to the more aggressive forms of multiple sclerosis. The more chronic active lesions a patient has the greater the chances they will experience this type of MS,” said Daniel S. Reich, senior investigator in the National Institute of Neurological Disorders and Stroke (NINDS) and the senior author of the paper with the results published in JAMA Neurology. “We hope these results will help test the effectiveness of new therapies for this form of MS and reduce the suffering patients experience.”
Affecting more than 2 million people worldwide, multiple sclerosis is a disease for which there is no cure. The disease starts when the immune system attacks myelin—a protective coating around nerve cells in a person’s brain and spinal cord—and produces a variety of initial symptoms, including blurred or double vision; problems with muscle strength, balance, and coordination; and abnormal sensations. Treatment with anti-inflammatory medications designed to quiet the immune system has helped some patients fully or partially recover. Nevertheless, a significant subset of patients will eventually suffer from a longer lasting, progressive form of the disease that can cause further problems including paralysis, loss of bladder control, and problems with attention, thinking, and memory.
Doctors often use magnetic resonance imaging (MRI) to diagnose the disease because the immune system’s attack produces lesions that appear as spots on scans of patients’ brains. While some of the lesions heal, completely or partially, other lesions remain and rimmed ones appear to actively expand, or “smolder,” for many years. Until recently, researchers did not fully understand the role chronic active lesions play in the disease, in part because it was difficult to find the ones that remain chronically inflamed.
Starting in 2013, Reich’s team showed that by using a high-powered, 7-tesla MRI scanner, they could accurately identify damaging, chronic active lesions by their darkened outer rims, in agreement with previous studies. (J Clin Invest 126:2597–2609, 2016; DOI:10.1172/JCI86198)
“Figuring out how to spot chronic active lesions was a big step and we could not have done it without the high-powered MRI scanner provided by the NIH. It allowed us to then explore how MS lesions evolved and whether they played a role in progressive MS,” said NINDS postdoctoral fellow Martina Absinta, of Reich’s lab, who performed these studies.
The team scanned the brains of 192 MS patients who had entered a trial at the NIH’s Clinical Center. The researchers found that, regardless of the treatment being received, 56% of the patients had at least one rimmed lesion. Further analysis showed that 44% of patients had only rimless lesions; 34% had one to three rimmed lesions; and 22% had four or more rimmed lesions.
The researchers then compared the brain scans to the neurological examinations the patients received upon enrollment. Patients who had four or more rimmed lesions were 1.6 times as likely to be diagnosed with progressive MS as those without rimmed lesions. Moreover, these patients developed motor and cognitive disabilities at a younger age than the patients who had no rimmed lesions. When the researchers analyzed key parts of the patients’ brains, they found that patients who had four or more rimmed lesions had less white matter and smaller basal ganglia than those who had no rimmed lesions.
“Our results point the way toward using specialized brain scans to predict who is at risk of developing progressive MS,” said Reich.
The team then analyzed a subset of patients whose brains had been scanned once every year for 10 years or longer. Their results suggested that, although the rimless lesions generally shrank, the rimmed lesions either grew or stayed the same size and were particularly damaged.
Finally, the team used a 3-D printer to compare the spots they had seen on scans with the lesions they observed in brain-tissue samples autopsied from a patient who had passed away during the trial. They found that all expanding rimmed spots seen on the scans had the telltale features of chronic active lesions when examined under a microscope.
“Our results support the idea that chronic active lesions are very damaging to the brain,” said Reich. “We need to attack these lesions as early as possible. The fact that these lesions are present in patients who are receiving anti-inflammatory drugs that quiet the body’s immune system also suggests that the field of MS research may want to focus on new treatments that target the brain’s unique immune system–especially a type of brain cell called microglia. At the NIH, we are actively seeking patients who want to participate in studies like these.”
In a previous article, Reich’s team openly shared instructions for programming lower-powered MRI scanners, found at most clinics, to detect rimmed chronic active lesions. The team hopes that researchers around the world will use the instructions to develop and monitor better diagnostic and therapeutic strategies for MS patients.
(NIH authors: M. Absinta, P. Sati, F. Masuzzo, G. Nair, V. Sethi, H. Kolb, J. Ohayon, T. Wu, I.C.M. Cortese, and D.S. Reich, JAMA Neurol, August 12, 2019; DOI:10.1001/jamaneurol.2019.2399). These studies were supported by the NINDS Intramural Research Program, the National Multiple Sclerosis Society, and the Conrad N. Hilton Foundation.
This page was last updated on Thursday, March 31, 2022
