Research Briefs
NEI: IMMUNE SYSTEM CAN SLOW DEGENERATIVE EYE DISEASE
CREDIT: NEI
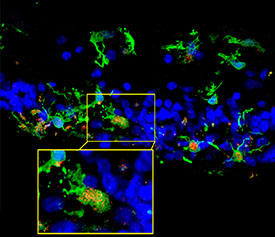
Retinal sections from a patient with retinitis pigmentosa show microglia (green) migrating into the photoreceptor layer (blue) after degeneration began. Inset shows microglia expressing C3 (red), which occurred in the context of photoreceptor degeneration. C3 is the central component of complement, and its absence made degeneration worse.
A new study, conducted by NEI scientists, shows that the complement system, part of the innate immune system, plays a protective role in slowing retinal degeneration in a mouse model of retinitis pigmentosa, an inherited eye disease. This surprising discovery contradicts previous studies of other eye diseases—such as age-related macular degeneration—that suggest the complement system worsens retinal degeneration. The current study shows, however, that in the context of retinitis pigmentosa, complement activation is actually helpful for clearing away dead cells and maintaining homeostasis, a physiological balance, in the retina.
Using the retinitis pigmentosa mouse model, the researchers examined the role of C3 and CR3, the central component of complement and its receptor, by comparing mice with genetically ablated genes C3 or CR3 to mice with normal expression. They found that the absence of the genes made degeneration worse.
Further research is needed to complete the picture of how, and under what circumstances, complement activation has beneficial or harmful effects on photoreceptors and disease progression. (NIH authors: S.M. Silverman, W. Ma, Z. Wang, L. Zhao, and W.T. Wong, J Exp Med 2019; DOI:10.1084/jem.2019000)
NIAID: SCIENTISTS DEVELOP “MINI-BRAIN” MODEL OF HUMAN PRION DISEASE
CREDIT: NIAID
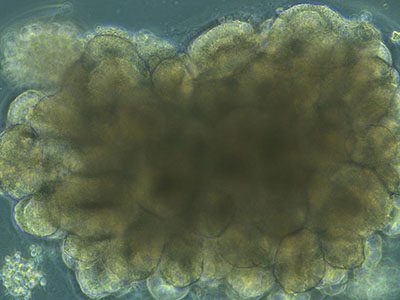
Bright-field microscope image of an organoid during development, showing highly structured regions forming.
NIAID scientists at Rocky Mountain Laboratories (Hamilton, Montana) have used human skin cells to create what they believe is the first cerebral organoid system, or “mini-brain,” for studying sporadic Creutzfeldt-Jakob disease (CJD). CJD is a fatal neurodegenerative brain disease of humans believed to be caused by infectious prion proteins. CJD affects about 1 in 1 million people. The researchers hope the human organoid model will enable them to evaluate potential therapeutics for CJD and provide greater detail about human prion disease subtypes than the rodent and nonhuman primate models currently in use.
In this study, the researchers discovered how to infect five-month-old cerebral organoids with prions using samples from two patients who died of two different CJD subtypes, MV1 and MV2. Infection took about one month to confirm, and the scientists monitored the organoids for changes in health indicators, such as metabolism, for more than six months. By the end of the study, the scientists observed that seeding activity, an indication of infectious prion propagation, was present in all organoids exposed to the CJD samples. However, seeding was greater in organoids infected with the MV2 sample than in the MV1 sample. They also reported that the MV1-infected organoids showed more damage than the MV2-infected organoids.
Ultimately, the scientists hope to learn how to prevent cell damage and to restore the function of cells damaged by prion infection. The new system also provides opportunities to test potential therapeutics for CJD in a tissue model that mimics the human brain. (NIH authors: B.R. Groveman, S.T. Foliaki, C.D. Orru, J.A. Carroll, B. Race, and C.L. Haig, Acta Neuropathol Commun 7:12, 2019; DOI:10.1186/s40478-019-0742-2)
NICHD: BEING TEASED ABOUT WEIGHT MAY LEAD TO MORE WEIGHT GAIN AMONG CHILDREN
Youth who said they were teased or ridiculed about their weight increased their body mass by 33 percent more each year than a similar group who had not been teased, according to researchers at NICHD and the Uniformed Services University of the Health Sciences (Bethesda, Maryland). The findings appear to contradict the belief that such teasing might motivate youth to change their behavior and attempt to lose weight.
The study involved 110 youth who were an average of 11.8 years of age when they enrolled. The participants were either overweight as defined by the body-mass index when they began the study or had two parents who were overweight or obese. At enrollment, they completed a six-item questionnaire on whether they had been teased about their weight. They then participated in annual follow-up visits for the next 15 years. The researchers found that youth who experienced high amounts of teasing gained an average of 0.44 pounds per year more than those who did not. The authors theorize that weight-associated stigma may have made youths more likely to engage in unhealthy behaviors, such as binge eating and avoiding exercise. Another possible explanation is that the stress of being teased could stimulate the release of the hormone cortisol, which may lead to weight gain. (NIH authors: N.A. Schvey, S.E. Marwitz, S.J. Mi, O.A. Galescu, M.M. Broadney, D. Young-Hyman, S.M. Brady, J.C. Reynolds, M. Tanofsky-Kraff, S.Z. Yanovski, and J.A. Yanovski, Pediatr Obes May 29:e12538, 2019; DOI:10.1111/ijpo.12538)
NIDDK, CC, NINR: HEAVILY PROCESSED FOODS CAUSE OVEREATING AND WEIGHT GAIN

CREDIT: JENNIFER RYMARUK, NIDDK
Dietitians at the NIH Clinical Center designed recipes to test the effects of ultraprocessed and unprocessed diets on study participants.
People eating ultraprocessed foods ate more calories and gained more weight than when they ate a minimally processed diet, according to results from a study conducted by NIDDK researchers. The difference occurred even though meals provided to the volunteers in both the ultraprocessed and the minimally processed diets had the same number of calories and macronutrients.
This small-scale study of 20 healthy adult volunteers (10 males and 10 females) is the first randomized controlled trial to examine the effects of ultraprocessed foods as defined by the NOVA classification system. This system considers foods “ultra-processed” if they have ingredients predominantly found in industrial food manufacturing, such as hydrogenated oils, high-fructose corn syrup, flavoring agents, and emulsifiers.
Previous observational studies looking at large groups of people had shown associations between diets high in processed foods and health problems. But, because none of the past studies randomly assigned people to eat specific foods and then measured the results, scientists could not say for sure whether the processed foods were a problem on their own, or whether people eating them had health problems for other reasons, such as a lack of access to fresh foods.
For the study, researchers admitted the 20 volunteers to the NIH Clinical Center for one continuous month and, in random order for two weeks on each diet, provided them with meals made up of ultraprocessed foods or meals of minimally processed foods. The ultraprocessed and unprocessed meals had the same amounts of calories, sugars, fiber, fat, and carbohydrates, and participants could eat as much or as little as they wanted.
On the ultraprocessed diet, people ate about 500 calories more per day than they did on the unprocessed diet. They also ate faster on the ultraprocessed diet and gained weight, whereas they lost weight on the unprocessed diet. On average, participants gained about two pounds while they were on the ultraprocessed diet and lost an equivalent amount on the unprocessed diet.
The researchers plan to design similar studies with a reformulated ultraprocessed diet to see whether the changes can make the diet effect on calorie intake and body weight disappear. For example, slight differences in protein amounts between the two diets could potentially explain as much as half the difference in calorie intake.
While the study reinforces the benefits of unprocessed foods, researchers note that ultraprocessed foods can be difficult to restrict and that some people don’t have easy access to healthy foods. (NIH authors: K.D. Hall, A. Ayuketah, R. Brychta, H. Cai, T. Cassimatis, K.Y. Chen, S.T. Chung, E. Costa, A. Courville, V. Darcey, L.A. Fletcher, A.M. Gharib, J. Guo, R. Howard, P.V. Joseph, S. McGehee, R. Ouwerkerk, K. Raisinger, I. Rozga, M. Stagliano, M. Walter, P.J. Walter, S. Yang, and M. Zhou, Cell Metab 30:1–11, 2019; DOI:10.1016/j.cmet.2019.05.008)
NIEHS: SLEEPING WITH ARTIFICIAL LIGHT AT NIGHT ASSOCIATED WITH WEIGHT GAIN IN WOMEN
Sleeping with a television or light on in the room may be a risk factor for gaining weight or developing obesity, according to scientists at NIEHS. The research is the first to find an association between any exposure to artificial light at night while sleeping and weight gain in women. The results suggest that cutting off lights at bedtime could reduce women’s chances of becoming obese.
The research team used questionnaire data from 43,722 women in the Sister Study, a cohort study that examines risk factors for breast cancer and other diseases. The participants, aged 35 to 74 years, had no history of cancer or cardiovascular disease and were not shift workers, daytime sleepers, or pregnant when the study began. The study questionnaire asked whether the women slept with no light, a small nightlight, light outside of the room, or a light or television on in the room.
The scientists used weight, height, waist and hip circumference, and body mass index measurements taken at baseline, as well as self-reported information on weight at baseline and follow-up five years later. Using this information, the scientists were able to study obesity and weight gain in women exposed to artificial light at night compared with women who reported sleeping in dark rooms.
The results varied with the amount of exposure to artificial light at night. For example, using a small nightlight was not associated with weight gain, whereas women who slept with a light or television on were 17 percent more likely to have gained approximately 11 pounds or more over the follow-up period. The association with having light coming from outside the room was more modest.
Also, the scientists wondered if not getting enough rest factored into the findings. They acknowledge that other confounding factors could explain the associations between artificial light at night and weight gain. However, their findings did not change when analyses controlled for characteristics that may be associated with exposure to light at night. These factors included age, having an older spouse or children in the home, race, socioeconomic status, calories consumed, and physical activity. (NIH authors: Y.-M.M. Park, A.J. White, C.L. Jackson, C.R Weinberg, and D.P. Sandler, JAMA Intern Med 2019; DOI:10.1001/jamainternmed.2019.0571)
NCI: STUDY SHOWS INCIDENCE OF AGGRESSIVE SUBTYPES OF UTERINE CANCER RISING
CREDIT: NCI
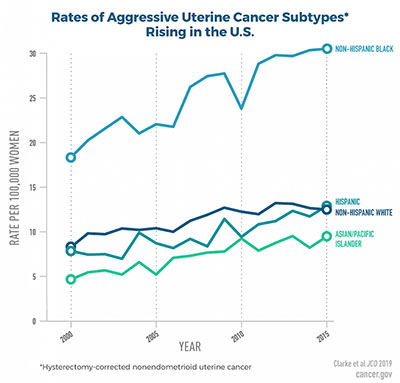
Rates of aggressive uterine cancer subtypes rising in the United States.
New findings from a study by researchers at NCI show that U.S. incidence (rate of new cases of a disease during a span of time) for aggressive subtypes of uterine cancer rose rapidly among women ages 30 to 79 from 2000 to 2015. The findings also reveal racial disparities including higher incidence of these aggressive subtypes and poorer survival—irrespective of subtype and cancer stage—among non-Hispanic black women than among women in other racial and ethnic groups.
The study used population data from NCI’s Surveillance, Epidemiology, and End Results (SEER) database to evaluate trends in uterine cancer incidence rates for women overall and by race and ethnicity, geographic region, and histologic subtype (subtypes differentiated by how tumor tissue appears under a microscope). The authors corrected for hysterectomy prevalence (the proportion of a population with a condition), using data from the Behavioral Risk Factor Surveillance System, in estimating incidence of uterine cancer because women who have had a hysterectomy are no longer at risk for developing the disease. Many past studies of uterine cancer incidence did not include such a correction.
The study found that, among all women, hysterectomy-corrected uterine cancer incidence overall increased by about one percent per year from 2003 to 2015. Incidence increased more rapidly among women of other racial and ethnic groups than among white women. Uterine cancer incidence rates among black women surpassed that among white women in 2007 and were consistently higher from 2011 through 2015.
“We need to continue research to further understand these racial differences and disparities, in order to help us better predict risk and work toward prevention,” said Megan Clarke, lead author of the study and a postdoctoral fellow in NCI’s Division of Cancer Epidemiology and Genetics. (NIH authors: M. Clarke, S.S. Devesa, S.V. Harvey, and N. Wentzensen, J Clin Oncol, 2019; JCO.19.00151)
NIAID: EXPERIMENTAL DRUG COMPLETELY EFFECTIVE AGAINST NIPAH VIRUS INFECTION IN MONKEYS

CREDIT: NIAID
Scanning electron micrograph of Nipah virus (yellow) budding from the surface of a cell.
The experimental antiviral drug remdesivir completely protected four African green monkeys (Chlorocebus sabaeus) from a lethal dose of Nipah virus, according to a new study from scientists at NIAID’s Rocky Mountain Laboratories (Hamilton, Montana) and collaborators at the Centers for Disease Control and Prevention (Atlanta), and Gilead Sciences (Foster City, California).
First identified in 1999 in Malaysia, Nipah virus is an emerging pathogen found primarily in Bangladesh and India. The virus is spread to humans by fruit bats (genus Pteropus and suborder Microchiroptera); person-to-person transmission also occurs. Nipah virus can cause neurological and respiratory disease; the mortality rate is about 70 percent. Delayed relapse, manifesting as brain inflammation or encephalitis, can occur. An outbreak in May 2018 in India resulted in 23 cases and 21 deaths.
Animals infected with a lethal dose of Nipah virus received a first dose of intravenous remdesivir 24 hours after infection and then a daily intravenous dose for a total of 12 consecutive days. The NIAID team observed the animals for 92 days after infection. Two treated animals developed mild respiratory signs that resolved within three weeks; the other two treated monkeys showed no signs of illness. All four remained apparently healthy for the remainder of the study.
Scientists next plan to evaluate delayed drug administration to determine how long after infection the animals can be treated successfully. Remdesivir is the second experimental treatment, after monoclonal antibody m102.4, shown to prevent severe Nipah virus disease in a monkey model when administered after the animals are infected. (NIH authors: Friederike Feldmann, Jacqueline Cronin, Heinz Feldmann, and Emmie de Wit, Sci Transl Med 11:Issue 494, eaau9242, 2019; DOI: 10.1126/scitranslmed.aau9242)
This page was last updated on Monday, April 4, 2022
