Research Briefs
NIAMS, NHGRI, NCI: LINK BETWEEN GENE REGULATORY ELEMENTS AND AUTOIMMUNE DISEASES
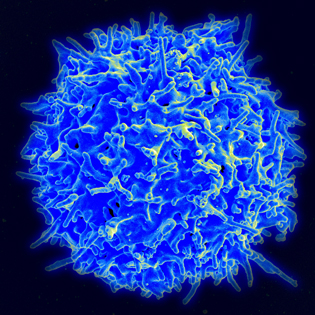
CREDIT: NATIONAL INSTITUTE OF ALLERGY AND INFECTIOUS DISEASES
NIAMS and other NIH investigators have discovered the genomic switches of a blood cell key to regulating the human immune system. Shown: Scanning electron micrograph of a human T lymphocyte from the immune system of a healthy donor.
NIH investigators have discovered the genomic switches of a blood cell key to regulating the human immune system. The findings open the door to new research and development in drugs and personalized medicine to help those with autoimmune disorders such as inflammatory bowel disease and rheumatoid arthritis. Genetic studies have shown that people with autoimmune diseases possess unique genetic variants, but most of the alterations are found in regions of the DNA that do not carry genes. Scientists have suspected that the variants are in DNA elements called enhancers, which act like switches to control gene activities.
The NIH researchers wondered whether the alterations might lie in a newly discovered type of enhancer called a super-enhancer (SE). Earlier work at NIH had shown that SEs are especially powerful switches and that they control genes important for the function and identity of individual cell types. In addition, many disease-associated genetic alterations were found to fall within SEs, suggesting that disease occurs when these switches malfunction. The team used genomic techniques to comb the T-cell genome for regions that are particularly accessible to proteins, a hallmark of DNA segments that carry SEs. Several hundred such regions were identified. Further analysis showed that they largely control the activities of genes that encode cytokine and cytokine receptors, which enable T cells to communicate with other cells and mount an immune response.
But the researchers’ most striking observation was that a large fraction of previously identified alterations associated with rheumatoid arthritis and other autoimmune diseases localized to these T-cell SEs. Additional experiments provided further evidence for a central role for SEs in rheumatoid arthritis. When the scientists exposed human T cells to tofacitinib, a drug used to treat rheumatoid arthritis, the activities of genes controlled by SEs were profoundly affected compared with other genes without SEs. This result suggests that tofacitinib may bring about its therapeutic effects in part by acting on SEs to alter the activities of important T-cell genes. (NIAMS: G. Vahedi, Y. Kanno, K. Jiang, J.J. O’Shea, Y. Furumoto, M. Gadina, and V. Sartorelli; NHGRI: S.C.J. Parker, M.R. Erdos, and F.S. Collins; NCI: S.R. Davis, R. Roychoudhuri, and N.P. Restifo, Nature DOI:10.1038/nature14154)
NIA: INSULIN RESISTANCE AS NOVEL BIOMARKER IN ALZHEIMER DISEASE
Researchers from the National Institute on Aging, working with scientists from four other organizations, have developed a blood test that shows that the brains of patients with Alzheimer disease (AD) do not respond normally to the action of insulin. Numerous epidemiological studies have shown that both type 2 diabetes (DM2) and insulin resistance are risk factors for AD. Many patients with AD exhibit reduced cerebral glucose metabolism similar to patients with DM2, making insulin resistance a contributing factor to the pathophysiology of AD. The researchers measured the blood levels of a phosphorylated form of a signaling protein called type 1 insulin receptor substrate (IRS-1) in neurally derived plasma exosomes. The samples came from 26 people with AD, 20 elderly cognitively normal individuals with DM2, 16 people with frontotemporal dementia (FTD), and matched case-control subjects.
In addition, the researchers tested blood samples obtained at two points from 22 individuals—at the time of diagnosis of AD and one to 10 years before when they were cognitively normal. The study showed that the concentrations of two factors—P-serine 312-IRS-1 and P-pan-tyrosine-IRS-1—as well as the ratio of these two factors, termed the insulin resistance index, were significantly different in patients with AD, DM2, and FTD than in the control subjects; were higher for patients with AD than for patients with DM2 or FTD; and accurately predicted the development of AD up to 10 years before clinical onset. The researchers say that if their findings are replicated in large, longitudinal controlled prospective studies, this test may be used for early diagnosis of AD and to measure responses to new treatments. (NIA authors: D. Kapogiannis, A. Biragyn, E.J. Goetzl; FASEB J 29:589–596, 2015)
NIDCD, NHLBI: PROTEIN LINKED TO A FORM OF HEREDITARY HEARING LOSS
For the first time, NIH researchers have purified a key part of myosin 15, a molecular motor protein that helps build healthy hearing structures in the inner ear. Mutations in the myosin 15 gene (MYO15A) have been linked to a form of hereditary deafness in humans. Using a novel approach to express the protein, the researchers revealed the first detailed insight into the molecule’s structure and function, laying the foundation for new treatments for some forms of hearing loss. The new approach to expressing myosin 15 may also help the study of other types of myosin motors, such as skeletal and cardiac muscle myosins, which could accelerate the development of targeted drug therapies for heart disease and other health conditions. (NIH authors: J.E. Bird, Y. Takagi, N. Billington, M.-P. Strub, J.R. Sellers, and T.B. Friedman, Proc Natl Acad Sci USA 111:12390–12395, 2014)
NIAAA: MANY AMERICANS AT RISK FOR ALCOHOL-MEDICATION INTERACTIONS
In the United States, nearly 42 percent of adults who drink also report using medications known to interact with alcohol, based on a recently released NIH study. Among those over 65 years of age who drink alcohol, nearly 78 percent report using alcohol-interactive medications. Such medications are widely used, prescribed for common conditions such as depression, diabetes, and high blood pressure.
The research is among the first to estimate the proportion of adult drinkers in the United States who may be mixing alcohol-interactive medications with alcohol. The resulting health effects can range from mild (nausea, headaches, loss of coordination) to severe (internal bleeding, heart problems, difficulty breathing). Older adults are particularly at risk for experiencing alcohol-medication interactions. Not only are they more likely to be taking medications in general, but also certain alcohol-interactive medications, such as diazepam (Valium), are metabolized more slowly as one ages, creating a larger window for potential interactions.
The researchers analyzed data from more than 26,000 adults ages 20 and older who participated in the National Health and Nutrition Examination Survey (1999–2010). The survey asks participants about alcohol use in the past year and prescription drug use in the past month. The main types of alcohol-interactive medications reported in the survey were blood-pressure medications, sleeping pills, pain medications, muscle relaxers, diabetes and cholesterol medications, antidepressants, and antipsychotics. (NIAAA authors: R.A. Breslow, C. Dong, A. White, Alcohol Clin Exp Res 39:371–379, 2015)
NHGRI, NCATS, OD: TACKLING THE THORNY SIDE OF GENE THERAPY
NIH investigators have uncovered a key factor in understanding the elevated cancer risk associated with the use of adeno-associated virus (AAV) as a gene-therapy vector. They conducted research on mice with a rare disease similar to one in humans, hoping their findings may eventually help improve gene therapy for humans. Toxic side effects are rarely observed by researchers who have designed gene therapies using an AAV as a vector to deliver the corrected gene to a specific point in a cell’s DNA. AAVs, small viruses that infect humans but do not cause disease, are uniquely suited for gene-therapy applications. But a prior study found an association between AAV and the occurrence of liver cancer.
The present research addresses this problem in gene therapy for an inherited disease in children called methylmalonic acidemia (MMA), which affects as many as one in 67,000 children born in the United States. Affected children are unable to properly metabolize certain amino acids, an inability that can damage several organs and lead to kidney failure. MMA patients also suffer from severe metabolic instability, failure to thrive, intellectual and physical disabilities, pancreatitis, anemia, seizures, vision loss, and stroke. The most common therapy is a restrictive diet, but doctors must resort to dialysis or kidney or liver transplants when the disease progresses.
In prior MMA gene-therapy studies, researchers showed that mice bred to develop the condition could be restored to health by AAV gene-therapy injection shortly after birth. These mice survived into adulthood and were free from the effects of MMA, but in a long-term follow-up after they reached about two years of age, the researchers documented a 50–70 percent higher occurrence of liver cancer in the AAV-treated mice compared with a 10 percent liver cancer rate in untreated mice. The scientists determined that the AAV vector triggered the cancer.
In additional experiments, the research team determined that in many mice that developed liver cancer, the AAV vector targeted a region of the mouse genome called Rian, near a gene called Mir341, which codes for a microRNA molecule. When the AAV was inserted near Mir341, the vector caused elevated expression of the gene, which the researchers believe contributed to the occurrence of liver cancer in the mice. Mir341 is found in the mouse genome; however, it is not present in humans.
When the researchers used an alternate AAV vector to deliver the corrected gene in a study of just 10 mice, that vector did not insert itself where it would elevate the expression of nearby genes, and it did not cause liver cancer. The researchers found that this modification made for a safer gene therapy and that lower doses of AAV resulted in reduced rates of liver cancer. The hope is that the methodologies described in their research will be used by others to study the toxicity of AAV vectors in preclinical trials. (NIH authors: R.J. Chandler, M.C. LaFave, G.K. Varshney, N.S. Trivedi, N. Carrillo-Carrasco, J.S. Senac, W. Wu, V. Hoffman, A.G. Elkahloun, S.M. Burgess, C.P. Venditti, J Clin Invest 125:870–880, 2015)
NIDDK: DISCOVERY PROVIDES INSIGHT INTO IMMUNITY
Using X-ray diffraction, researchers from the NIDDK Laboratory of Molecular Biology were the first to determine the crystal structure of the recombination-activating genes (RAG1-RAG2) protein complex. The complex initiates DNA recombination and rearrangement to generate a highly diverse population of antibodies and T-cell receptors that are needed to defend against infection. By knowing the structure of the complex, the scientists are able to explain more than 60 human mutations that lead to immune deficiencies. Their work has laid the groundwork for analyzing whether and how variations in RAG1 and RAG2 genes affect the diversity of antibodies in an individual and the implications for immune diseases. (NIDDK authors: M.S. Kim, M. Lapkouski, W. Yang, and M. Gellert, Nature 518:507–511, 2015)
NCATS, NICHD, CC: TEAMING WITH INDUSTRY TO DEVELOP TREATMENTS FOR NIEMANN-PICK DISEASE
Researchers from NIH have entered into an agreement with the biotechnology company Vtesse, Inc. (Gaithersburg, Maryland), to develop treatments for Niemann-Pick disease type C (NPC) and other lysosomal storage disorders. In lysosomal storage diseases, also known as lipid-storage diseases, fatty materials accumulate in the cells and tissues of the body. These diseases comprise about 50 rare inherited disorders that usually affect children. These diseases result in damage to the brain, peripheral nervous system, liver, and other organs and tissues, and are often fatal. Scientists at the National Center for Advancing Translational Sciences (NCATS) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) will conduct studies on NPC and other lysosomal storage disorders with funding provided by Vtesse. Vtesse will support the ongoing phase 1 clinical trial for NPC at the NIH Clinical Center, led by NICHD researchers who have been evaluating the safety of the drug cyclodextrin. Vtesse also plans to collaborate with NICHD to launch a second clinical study of cyclodextrin (anticipated to begin in 2015) for the treatment of NPC in the United States and Europe. The use of cyclodextrin for NPC has been granted orphan-drug designation in the United States and Europe, providing development incentives for products that demonstrate promise for the diagnosis and treatment of rare diseases or conditions. Researchers in NCATS’ Therapeutics for Rare and Neglected Diseases (TRND) program developed cyclodextrin as part of a project focused on finding treatments for NPC. The goal of TRND projects is to develop therapeutic candidates through a strategy known as de-risking, which involves the preclinical development of therapeutics to the stage at which they attract biotechnology and pharmaceutical companies such as Vtesse to invest in their further clinical development. (http://www.nih.gov/news/health/jan2015/ncats-07.htm)
NCCIH: SHIFTS IN AMERICANS’ USE OF NATURAL PRODUCTS
A nationally representative survey shows that natural product use in the United States has shifted since 2007, with some products becoming more popular and some falling out of favor. Overall, natural products (dietary supplements other than vitamins and minerals) remain the most common complementary health approach. A complementary health questionnaire was developed by NIH’s National Center for Complementary and Integrative Health (NCCIH) and the Centers for Disease Control and Prevention’s National Center for Health Statistics. The questionnaire is administered every five years as part of the National Health Interview Survey (NHIS), an annual study in which tens of thousands of Americans are interviewed about their health- and illness-related experiences. The 2012 NHIS survey is the most current, comprehensive, and reliable source of information on the use of complementary health approaches by adults and children in the United States. Survey highlights include:
- Fish oil was the top natural product among adults.
- Adults’ use of fish oil, probiotics or prebiotics, and melatonin increased between 2007 and 2012.
- Adults’ use of glucosamine and chondroitin, echinacea, and garlic decreased between 2007 and 2012.
- Fish oil was the top natural product among children. (In 2007, echinacea was first.)
- Melatonin was the second-most-used natural product by children in 2012.
Knowing the patterns of use of complementary approaches helps to inform NIH’s research priorities in this area. NCCIH’s research priorities also include the study of other complementary approaches—such as spinal manipulation, meditation, and massage—to manage pain and other symptoms that are not always well-addressed by conventional treatments. (https://nccih.nih.gov/research/statistics/NHIS/2012)
This page was last updated on Tuesday, April 26, 2022
