Brain Injuries
Detecting Them on the Battlefield
Imagine a handheld scanner that could be used in the battlefield to detect whether an injured soldier has suffered a traumatic brain injury (TBI). NICHD ’s senior investigator Amir Gandjbakhche and research fellow Jason Riley led a team of NIH scientists to perfect an imaging technology that would make such a device possible.
The idea was straightforward: Create a device that could detect a TBI and make it simple enough for any soldier to grab out of a truck and use it in the heat of battle. The device needed to be portable, able to withstand the chaos of the battlefield, and use an imaging technology that could measure bleeding in the brain, an emergency that requires immediate medical attention.
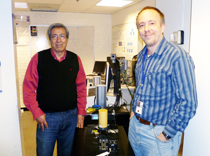
Alicia Evangelista, NHLBI
Amir Gandjbakhche (left) and Jason Riley (right) invented a portable device that might one day be used to detect traumatic brain injuries at accident scenes or on the battlefield.
Current imaging technology is sophisticated but limited. Magnetic resonance imaging and computed tomography scanners are large and unwieldy and therefore not very useful in the field. Near-infrared scanners, which use infrared light to detect hematomas, are portable, but the detection device must be held still to get accurate readings. Traditional imaging systems are based on mathematical models in which both the machine’s and the patient’s locations are fixed, but in the real world, things move, said Riley, a mathematician and engineer and the lead author of the paper that described a prototype hematoma detector (Biomed Opt Express 3:192–205, 2012).
Researchers at NIH’s Center for Neuroscience and Regenerative Medicine (CNRM), NINDS, NIBIB, CIT, and NICHD collaborated on a solution and figured out how to develop a motion-based sensor. The device employs a mathematical model that uses motion as a signal for detecting changes in blood volume in the head. Riley compared the technology to a global positioning system and the remote controls of gaming systems that track user motion. Inside the prototype, three motion lasers “talk” to one another, referencing their location in space compared with the other two sensors, thus tracking the movement of the device itself. Meanwhile, the device images the brain by using near-infrared light to penetrate the skull and characterizes the amount of blood pooling by measuring the changing light absorbance.
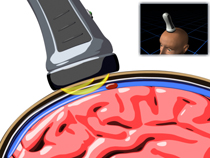
Tim Mzorek, NICHD
This prototype handheld near-infrared imaging device can be used at the scene of accidents to quickly detect traumatic brain injuries such as hematomas. To watch a video of the device in action, go to http://www.osa.org/About_Osa/Newsroom/News_Releases/Releases/12.2011/Monthly-Tip-Sheet-December-2011.aspx.
An existing handheld device called the InfraScanner—developed by the Office of Naval Research, approved recently by the Food and Drug Administration, and used in Europe—requires the user and patient to remain motionless. But the NIH device, a cross between a Star Trek tricorder and an electric razor, could move over the skull and use a motion signal to monitor light absorbance, pinpointing where the absorbance changes and identifying locations of pooled blood. In tests using optical phantoms (small objects mimicking the material properties of the skull), the prototype was able to successfully identify deposits of India ink that simulated hematomas.
Riley and Gandjbakhche have submitted a proposal to the NIH Bench-to-Bedside program to build a prototype that will be tested at Suburban Hospital (Bethesda, Md.). It could take five years before this low-cost device is ready for the battlefield. The researchers also envision a variety of other uses: in hospital emergency rooms for diagnosing hematomas quickly and effectively; in developing nations, where expensive diagnostic equipment is not available; and as a wireless device that would allow a user in a remote location to send brain images for assessment at a hospital far away.
The collaborators on this project include Gandjbakhche and Riley (NICHD); Eric Wassermann (NINDS); Paul Smith (NIBIB); Tom Pohida (CIT); and James Smirniotopoulos (CNRM, a collaborative of NIH and the Department of Defense to address TBI; see http://www.usuhs.mil/cnrm).
This page was last updated on Monday, May 2, 2022
