Here Come the Computers
NIH AI Symposium Highlights IRP Efforts to Harness Artificial Intelligence

IRP researchers are using AI-powered tools in many different ways to augment their efforts to improve human health.
Artificial intelligence is permeating seemingly every aspect of society — it’s even the villain in the latest Mission Impossible movie. Biomedical research is no exception to this trend, as showcased at this year’s NIH AI Symposium. The day-long event on May 16 showcased the many ways IRP researchers are harnessing the ever-growing learning capabilities of computers to explore how our bodies work and improve our health.
In between fascinating lectures by IRP senior investigators and visiting scholars from Harvard Medical School and the Massachusetts Institute of Technology, a handful of IRP postbaccalaureate fellows, graduate students, and postdocs also gave short talks about how their labs are utilizing AI and machine learning in their research. Read on to learn about how four of these efforts could one day help speed up therapeutic development for cancer and rare diseases, reveal the relationship between brain activity and behavior, and identify patients with sickle cell disease who would benefit the most from high-risk, intensive treatments.
Predicting the Fates of Sickle Cell Patients
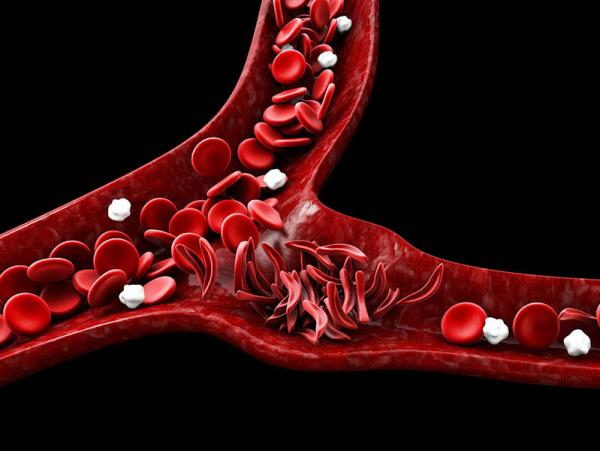
IRP researchers developed AI tools that can help doctors and patients more accurately predict the consequences of the blood cell traffic jams that occur in sickle cell disease.
It’s hard enough trying to figure out why one person develops a certain condition and another doesn’t, but once a person develops a disease, it can be just as difficult to predict the course it will take. Solving that problem would go a long way toward optimizing treatment for patients. After all, every treatment comes with side effects or other risks, and it would be unwise to give a patient an extremely debilitating or risky treatment if their condition was not truly life-threatening.
Thanks to a group of IRP researchers, those sorts of decisions might one day get easier for physicians treating sickle cell disease, a condition in which abnormally shaped red blood cells cause seemingly random traffic jams in blood vessels, causing severe pain and cutting off the life-sustaining supply of oxygen to organs. At this year’s NIH AI Symposium, Gefei Lin, a graduate student in statistics at George Washington University, related how he is working with several IRP researchers to develop an AI tool that can predict the likelihood that a person with sickle cell will die or that their condition will worsen. Such predictions would enable their doctors to make more informed decisions about when to recommend high-risk treatments like stem cell transplants.
“Sickle cell disease is well known for its extreme variability in disease course and outcome,” Gefei explains. “With the development of curative therapies that incur high risks, it has become increasingly important to develop a reliable decision tool for choosing patients eligible for disease-modifying or curative treatments.”
The AI approach Gefei is working on was developed in collaboration with researchers from the Sickle Cell Branch at NIH’s National Heart, Lung, and Blood Institute (NHLBI), led by IRP senior investigator Swee Lay Thein, F.R.C.P, D.Sc. The Branch’s clinical evaluations of hundreds of sickle cell patients provided the dataset that Gefei and his advisors in the NHLBI Office of Biostatistics Research used to train the AI algorithm. In the end, they were able to create a program that could use easily collectible health metrics to predict patients’ risk of death within the next five years with roughly 86 percent accuracy.
Now that the AI tool has been created and shown to provide useful predictions, Gefei’s team is working on creating a user-friendly online application allowing doctors and researchers to use their program. In addition, they want to figure out a way to more accurately determine how uncertain individual predictions made by the tool are so that doctors can better evaluate whether to take a certain prediction into account when making treatment decisions.
“We not only want to give an accurate prediction of the risk of death or progression of disease, but also inform patients and physicians how confident they can be in the result,” Gefei says.
Speeding Up the Search for Cancer Killers

By creating an AI tool that can predict how different experimental drugs affect cancer cells, IRP researchers hope to more efficiently identify treatments that show promise for slowing the growth of tumors.
Many researchers use AI and machine learning because such software can deal with massive troves of data more easily than humans. IRP graduate student Yoshitaka Inoue, on the other hand, is creating an AI tool to deal with the opposite situation: a relative lack of data about how cancer cells respond when they are exposed to each of the thousands of experimental drugs researchers might test on them.
To do so, Yoshitaka’s lab, led by IRP Stadtman investigator Augustin Luna, Ph.D., has partnered with IRP specialists in multiple fields to combine the power of two different AI algorithms Dr. Luna’s lab is developing. One of these algorithms incorporates information about how proteins in cells interact with one another, as well as data on the behavior of cells’ genes. The second algorithm utilizes a variety of other types of data, including information from established databases and the text of scientific publications, to predict how drugs might affect cells.
“While biology has a lot of data, often the areas where AI and machine learning have been most accurate have much more data of one single, consistent type than we have for this drug response prediction challenge,” Yoshitaka explains. “This is why we continue to explore ways to augment the available data with additional information, like the network of protein interactions. In a way, we are seeking to mirror how humans can generalize mental models of the world with fewer examples and communicate the details of those models to others — like how we can describe what a cat looks like even if we have not seen examples of every breed of cat.”
Of course, experimental drugs can affect cells in a huge number of different ways. That’s why, for now, Yoshitaka and his colleagues are focused specifically on developing an AI tool that can accurately predict how cancer cells will respond to drugs known to affect certain proteins. By doing so, they hope to use the algorithm to more efficiently identify treatments that can slow cancer cells’ growth. However, if fed the right kind of training data, their algorithm could potentially predict how a variety of non-cancerous cells might respond to different drugs, giving their approach applications in therapeutic development for a huge number of diseases aside from cancer.
“Our model seeks to predict sensitivity to many drugs that work in different ways in many different cancer types, providing a global model of cell perturbations by drugs,” Yoshitaka says. “Additionally, though we have not tried this, we believe that the framework may be generic enough to be usable in other research areas, even ones outside of biology, with appropriate data.”
Improving Therapeutic Development for Rare Diseases

AI can help researchers identify rare diseases that share a common cause, which could help them gather larger groups of patients for clinical trials of experimental therapies and get those treatments into the hands of patients more quickly.
Patients and policymakers alike often complain about how long it takes experimental therapies to become easily available to those who need them. This process is even more drawn out for rare diseases, since it takes so long to collect sufficient data on the sparse populations of people with such ailments.
One way to speed up this process is to use basket trials, in which a treatment that affects a certain biological process is tested in a group of patients whose diagnoses differ but whose symptoms are all caused at least in part by that single process. This makes it easier and faster to gather enough data about a drug’s effects to determine if it should move forward towards approval by the U.S. Food and Drug Administration (FDA). Determining which diseases all share a common cause, though, can make organizing basket trials difficult — which is where AI comes in.
Sungrim Moon, Ph.D., an IRP Data and Technology Advancement (DATA) Scholar, is working with several IRP colleagues to develop an AI tool that uses several types of biomedical, genetic, and other data from patients with a wide array of rare diseases to figure out which of those illnesses might share biological roots. Once their algorithm groups together ailments with such similarities, researchers can recruit patients with those diseases for a single basket trial rather than organizing a separate clinical trial for each of the identified illnesses.
“This approach aims to identify promising disease candidates for inclusion in basket trials, thereby facilitating more efficient and targeted therapeutic development in real-world settings,” Dr. Moon says.
And the approach doesn’t just sound good on paper. When provided with genetic data from individuals with a range of rare diseases, the IRP team’s algorithm grouped together diseases that had already been identified as possible candidates for shared basket trials, including conditions linked to mutations in the NLRP3 gene, which codes for a protein involved in the immune system. This suggests the algorithm may be useful for choosing disease candidates for basket trials based on molecular relationships scientists already know about. Interestingly, the algorithm also grouped together several diseases that are not yet well-understood or were not previously known to share underlying mechanisms, hinting at the potential of AI to uncover new relationships between diseases that scientists could explore.
“AI and machine learning offer powerful solutions by enabling the analysis of large, diverse datasets,” Dr. Moon explains. “These datasets are complex and high-dimensional, involving thousands of genes and mutations per patient. AI methods can manage the scale and complexity of such data, far beyond what would be feasible manually or through simple statistical approaches, especially given the non-linear and interdependent nature of biological data. They help detect subtle biological similarities and meaningful patterns that might be overlooked by human experts.”
The successes achieved by their AI algorithm so far are motivating Dr. Moon to continue refining it, such as by feeding it more types of data to help it select diseases to group together. In addition, she and her colleagues have so far only tested the algorithm using information about diseases caused by various different mutations in the same gene. To truly test the limits of their AI tool, they want to see how it groups diseases caused by mutations in different genes that affect the same biological process. And, of course, it remains to be seen whether basket trials designed with the assistance of AI truly help test the effectiveness of experimental treatments.
“Real-world implementation and prospective validation in clinical trials remain essential,” Dr. Moon says. “To fully realize the potential of this approach, AI-generated disease sub-clusters must be tested in actual basket trials. Ultimately, our goal is to develop a platform that routinely supports the design of smarter, faster, and more effective clinical trials by leveraging biological similarity rather than relying solely on traditional disease pathways.”
Adding AI to Brain and Video Recordings

In some NIH clinical studies, participants’ brain activity is monitored constantly for days or weeks. Combining that data with video footage and adding a dose of AI could yield interesting insights into what participants brains’ are doing while participants are eating, sleeping, or engaging in other activities during their hospital stays.
Some IRP clinical studies only require patients to visit the NIH Clinical Center for an hour or a day, but patients with epilepsy may stay there for up to two weeks while researchers led by IRP senior investigator Kareem Zaghloul, M.D., Ph.D., monitor their brains to learn about the source of their seizures. That’s a lot of down time, so it’s no wonder that his team is using AI to make maximum use of it.
Fortunately, patients in his team’s clinical studies are observed by video cameras 24-7 for their safety, and AI has proven that it does a great job of figuring out what is going on in an image or snippet of film. Consequently, Dr. Zaghloul’s team is combining two AI algorithms to create software that automatically notes what a patient is doing at any given time during their stay at the Clinical Center. The first algorithm, called a ‘pose model’ figures out where the various parts of a patients’ body are in space, and the second, called a ‘classifier model,’ uses that information to classify what a patient is doing.
“If we can know for certain from AI what is happening in a video, we can take advantage of the neural recordings we have for the possibility of researching and advancing our understanding of the human brain,” says IRP postbaccalaureate research fellow Caroline Maclaren, who gave a presentation about the project at the AI Symposium.
So far, the AI tool can tell whether a patient is eating or drinking, laying down, sitting up, or using their phone. While still in the exploratory phase, it provides a highly accurate proof-of-concept that the system could be further developed in order to identify activities or behaviors that are more interesting to researchers. For instance, if the AI tool can be taught to detect a wider array of behaviors, including when a patient is having a seizure, Dr. Zaghloul’s team can analyze the data to see if there are patterns in what patients are doing shortly before their seizures. Such an analysis might eventually yield a way to predict seizures before they happen based on patients’ behavior. And even the current, preliminary version could be combined with the IRP researchers’ brain recordings so they can explore what participants’ brains are doing when they’re sleeping, scrolling the Internet on their phones, or eating.
“There are a lot of opportunities,” Caroline says. “The main purpose of this AI tool is to really tap into that data that we aren’t currently using. If we can effectively do that, we can open new research questions for our lab.”
Subscribe to our weekly newsletter to stay up-to-date on the latest breakthroughs in the NIH Intramural Research Program.
Related Blog Posts
This page was last updated on Wednesday, June 11, 2025
