Have You Heard? Hearing Aids Reduce Cognitive Decline
Frank Lin’s WALS Lecture on Hearing Interventions and Brain Health
BY MEAGAN MARKS, NIAAA

CREDIT: COCHLEAR CENTER FOR HEARING AND PUBLIC HEALTH
Frank Lin is a clinician and researcher who regularly advocates policy changes that affect hearing issues. Here, he is pictured testifying in front of Congress in May 2017.
Thirty years ago, Frank Lin attended his first Wednesday Afternoon Lecture Series (WALS) event. A high school summer intern then, he nodded off at the recitation of high-level science so dense to his young ears. But on Nov. 15, Lin was on the other side of the WALS podium, presenting his own groundbreaking discoveries in otology and discussing the use of hearing aids to slow cognitive decline.
“If I have one goal for today, it is for no one to fall asleep,” joked Lin.
A lot has changed over the past three decades when it comes to the science of hearing loss, said Lin, who now serves as director of the Cochlear Center for Hearing and Public Health and professor of otolaryngology, medicine, mental health, and epidemiology at Johns Hopkins School of Medicine and Bloomberg School of Public Health (Baltimore).
Epidemiological research led by Lin and others, for example, has established the link between hearing loss and risk of dementia, but whether hearing intervention could reduce this risk was unknown. This question was clarified with the publication this year of the Aging and Cognitive Health Evaluation in Elders, or ACHIEVE, study, which found that cognitive decline may be slowed by hearing interventions in some senior cohorts. The ACHIEVE study, which is funded in part by NIA and led by Lin’s team, spans four research sites across the United States. The study recruited 977 adults ages 70–84 with untreated mild-to-moderate hearing loss. The ACHIEVE study stems from the Atherosclerosis Risk in Communities (ARIC) Neurocognitive Study, which set out to investigate cognitive impairment from midlife vascular risk factors. A portion of the participants (n = 238) from the ARIC study and other healthy community volunteers (n = 739) make up the two cohorts of the ACHIEVE study who have been followed since 2018.
Among the ARIC cohort, the ACHIEVE study’s hearing interventions reduced by 48% global and domain-specific cognitive decline. The strongest association was within the language domain.
Hearing interventions may also affect brain structure. Lin’s latest exploratory research findings support previous research that hearing loss could lead to structural atrophy, or thinning, of the brain as well as functional changes. Peripheral auditory input activates neural activity, he explained. Neural activity is a networked system that operates across regions of the brain. But what is not yet known is whether long-term hearing interventions, such as the use of hearing aids, can help to reduce those functional or structural changes over time. Lin’s research suggests it can.
His ACHIEVE study team examined cortical thinning via magnetic resonance imaging (MRI) scans at recruitment and at three years, and in the hearing intervention group, a 0.01 mm difference was measured in the frontal lobe as well as variations in thinning across the temporal, occipital, and parietal lobes.
“These very exploratory MRI results generally indicate a trend toward hearing intervention being associated with reduced cortical thinning,” Lin said. “I will be perfectly honest, when we did these analyses, we did not think we would see anything. I mean, three years is not much time, and yet there seems to be a signal that the hearing aid is doing something to the brain.”
Collectively, these patterns suggest that hearing interventions may result in sustained alterations of neural structure and activity. The potential mechanisms of this association could include direct or indirect effects, he cautioned. For example, it could be the enhancement of the sense of hearing that is affecting the brain, or it could be that enhanced hearing is allowing the individual to increase social and/or physical activity and that, theoretically, is what is affecting the brain structure.
Either way, hearing loss is something that is modifiable and treatable in late life. “That is why this is really important,” he said.
Noteworthy is the fact that Lin’s work has led to improved policies and the creation of technological standards. Over the years, he has worked with policymakers and testified before Congress to aid in the passage of the 2017 Over-the-Counter Hearing Aid Act, which opened the market for competitive innovation, made the United States the first country in the world to create a regulated hearing aid market, and made hearing aids more accessible to the millions of Americans with hearing loss.
Watch Frank Lin's Congressional testimony.
Lin also worked with the Consumer Technology Association to establish a standard testing methodology for a consumer-facing hearing metric (see sidebar) and to set common terminology to describe hearing wellness throughout a consumer’s lifetime.
The hearing interventions offered in the ACHIEVE study, which includes hearing aids and audiologist visits, are not covered under conventional Medicare insurance provisions.. Lin continues to advocate for this change.
The WALS talk featuring Lin is available on VideoCast at https://videocast.nih.gov/watch=51173. Researchers of all ages attended, and all appeared to remain wide awake.
Know Your Number
Mild to moderate hearing loss affects two-thirds of people over age 60.
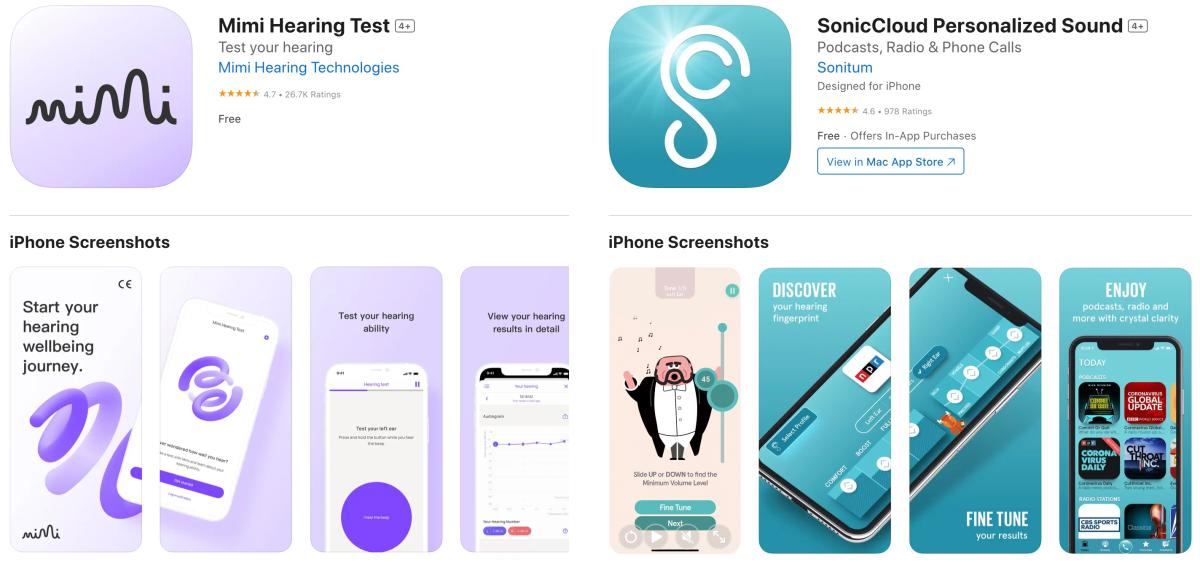
The NIH Catalyst staff downloaded and used these smartphone applications and tested our own hearing. According to the SonicCloud app, our new editor cannot hear the letter F. Do with that what you will….
“It doesn’t matter who you are, me or you, our hearing is going to decline as we get older,” Lin said during his WALS lecture. “It’s just the way humans are built.”
Even though hearing aids are becoming more accessible, there is still one foundational issue, according to Lin: Hearing is rarely tested.
“I’m guessing for most people in this room, you might have gotten your hearing measured when you were six or seven, in primary school,” Lin said during his presentation. “Yet, for the average American, you will never have your hearing tested again until you’re 80 years old and your spouse is screaming at you to get your hearing tested because you can’t hear what they are saying.
“My fundamental goal is for every teenager and adult around the world to understand, measure, and track their own hearing because enabling consumers to have access to health metrics (e.g., step count) can change behaviors at an unprecedented scale.”
Lin suggested visiting https://hearingnumber.org/ to learn what a Hearing Number is and how to track it. He has worked with technology companies such as Mimi and SonicCloud which create applications for Apple’s iOS platform for individuals to test their hearing and learn their Hearing Number.
“You do not need to see an [otolaryngologist] or an audiologist to know your Hearing Number. Just do it yourself, using your smartphone, and track it over time,” said Lin, who recommends individuals test their hearing at least once a year.
“Everything we do on a daily basis is related to communicating and hearing. Being able to monitor that over your lifetime and adapt technology strategies so you can always hear and communicate…well, it is sort of a no-brainer.”

Meagan Marks is a postbaccalaureate fellow in David Lovinger’s Laboratory for Integrative Neuroscience at NIAAA, where she studies motivation and reward. In her spare time, she enjoys exercising, playing the guitar, and exploring the D.C. area.
This page was last updated on Saturday, November 23, 2024
