Research Briefs
NHGRI, NIDCD, NCI: CERTAIN GENE MUTATIONS MAY CAUSE MELANOMA
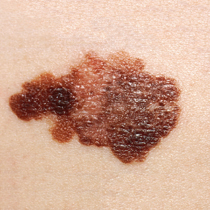
Melanoma on a patient ’s skin. (NCI)
Scientists have had little success in their search for an effective, long-lasting treatment for metastatic melanoma, a common form of skin cancer that is often fatal once it has spread. An NIH-led team of researchers has found that mutations in the gene for metabotropic glutamate receptor–3 (GRM3) cause some cases of the cancer. A biochemical analysis of GRM3 alterations revealed that mutant GRM3 selectively regulated the phosphorylation of a protein kinase called MEK. Melanoma cells expressing mutant GRM3 had reduced cell growth and cellular migration after treatment with a selective MEK inhibitor, AZD-6244, which is currently being used in phase 2 clinical trials. Further investigation into the mechanisms of GRM3 activation of the MEK pathway is needed, but the study suggests that targeting MEK signaling in the presence of GRM3 mutations may have a role in the treatment of melanoma. (NIH authors: T.D. Prickett, X. Wei, I. Cardenas-Navia, J.K. Teer, V. Walia, J. Gartner, J. Jiang, P.F. Cherukuri, A. Molinolo, S. A. Rosenberg, E.H. Margulies, Y. Samuels; Nat Genet 43:1119–1126, 2011)
NIDCD: DISCOVERY MAY ACCELERATE ADVANCES IN TREATING HEARING LOSS
A multi-institutional team, led by scientists at NIDCD and Harvard Medical School’s Children’s Hospital in Boston, has identified two proteins that may be the key components of the mechanotransduction channel in the inner ear. The channel is where the mechanical stimulation of sound waves is transformed into electrical signals that the brain recognizes as sound. The study used mice in which two genes, TMC1 and TMC2, had been deleted. The team observed that TMC2 knockout mice had normal hearing, but mice with no functional copies of TMC1 or TMC2 had the classic behaviors of dizzy mice—head bobbing, neck arching, unstable gait, and circling movements—and they were deaf. The TMC1 knockout mice were also deaf but they had no problem with balance. The team will continue to explore how TMC1 and TMC2 interact with each other and with other proteins. The genes may prove to be useful tools to screen for drugs or molecules that bind to the channel and could be used to prevent damage to hair cells. (NIDCD authors: Y. Kawashima, K. Kurima, V. Labay, T. Makishima, D.K. Wu, A.J. Griffith; J Clin Invest 121:4796–4809, 2011)
NIEHS: POTENTIAL NEW AVENUE FOUND FOR CANCER THERAPIES
Cancer can trick the body into producing new blood vessels to feed tumors. Vascular endothelial growth factor (VEGF) is known to play a role, but a team of researchers from NIEHS and several other institutions were the first to show that small molecules known as epoxyeicosatrienoic acids (EETs) are involved, too. VEGF and EETs work in concert to promote the spread of cancer by encouraging the growth of blood vessels that supply nutrients to the cancer cells. The findings suggest that blocking the production of EETs may eliminate the blood vessels that feed the tumors and this procedure could represent a novel strategy for treating cancer. To find out how EETs encourage the development of cancer, the team created two strains of mice, one with high levels of EETs and one with low levels. The mice with higher levels developed more metastatic tumors than did the mice with lower levels. The researchers determined that novel agonists such as 14,15-epoxyeicosa-5(Z)-enoic acid (EEZE), which is structurally similar to EET, block the effect of EETs and dramatically slow tumorigenesis in mice. EEZE, however, has not been approved for human use and is only used for research. (NIEHS authors: M.L. Edin, C.R. Lee, F.B. Lih, K.B. Tomer, D.C. Zeldin; J Clin Invest 122:178–191, 2012)
NCI: NEW KIND OF LIGHT THERAPY DESTROYS JUST CANCER CELLS
Photodynamic therapy can kill cancer cells, but it can damage normal cells, too. NCI researchers have designed a new type of light-based therapy that allows the selective destruction of tumor cells in mice without harming surrounding normal tissue. The new method could theoretically work against tumors in humans, such as those of the breast, lung, and prostate as well as cancer cells in the blood such as leukemias. The researchers developed a photoimmunotherapy (PIT) that couples a monoclonal antibody (MAb), which recognizes specific proteins on the surface of cancer cells, with a photosensitizer molecule that, when exposed to light of the appropriate wavelength (near-infrared), rapidly damages cells. It turned out that a near-infrared fluorescent dye called IR700 had the most favorable chemical properties. Photoimmunotherapy using MAb-IR700, unlike conventional photosensitizers, which can cause damage to healthy tissue, does not appear to harm normal cells. The study also found that antibody doses required for diagnosis were significantly lower than those required for therapy. Nevertheless, after MAb-IR700 exposure, the targeted tumors decreased in size and eventually disappeared, suggesting a potential means of controlling cancers with far lower doses of MAb than are usually administered to cancer patients. Because the MAb-IR700 compound also emits a small amount of light, it can be used to monitor therapy as well. Although more testing will be needed, the scientists believe the PIT method has the potential to replace some surgical, radiation, and chemotherapy treatments. (NCI authors: M. Mitsunaga, M. Ogawa, N. Kosaka, L.T. Rosenblum, P.L. Choyke, H. Kobayashi; Nat Med 17:1685–1691, 2011)
This page was last updated on Monday, May 2, 2022
