Catalytic Research
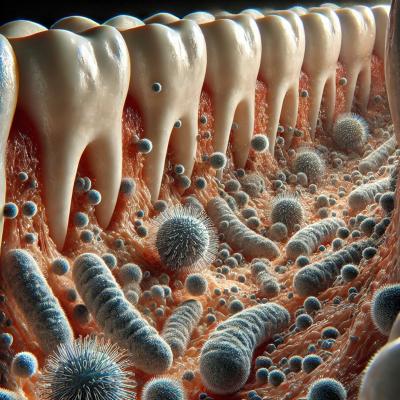
NIEHS, NCI, and CC researchers explored the association among sleep and the oral microbiome.
NIEHS, NCI, CC: SHORTER SLEEP LINKED TO DISRUPTIONS IN THE ORAL MICROBIOME
Your energy levels may not be the only thing suffering from lack of sleep—so may the vast microbial community co-existing in your body. According to a new NIH study, sleeping less than the recommended seven to eight hours a night is associated with reduced oral microbial diversity and distinct shifts in the types of bacteria present in the mouth.
Researchers at NIEHS and NCI compiled data from 1,139 older adults enrolled in the NIH-AARP Diet and Health Study. The team analyzed oral wash samples using 16S rRNA gene sequencing, a technique that can identify and compare bacteria from microbiome samples, to assess bacterial diversity and composition in relation to self-reported sleep duration.
The results suggest individuals who self-reported sleeping six hours or less per night had consistently lower microbial diversity in their mouths than those who slept the recommended seven to eight hours. These shorter sleepers also showed differences in certain families of bacteria. Specifically, they were found to have lower amounts of Prevotella and Corynebacterium–common commensal organisms in the mouth–and higher amounts of Streptococcus and Rothia. This finding persisted even after accounting for lifestyle factors such as smoking, neighborhood, and physical activity.
Although previous studies have focused on the gut microbiome, this study is the first of its kind to center on the role of the oral microbiome in sleep in healthy adults. It also uniquely accounted for the potential impact of lifestyle and neighborhood factors on associations with sleep and the oral microbiome.
The results of this study add to a growing body of evidence implicating the microbiome in the mediation of health consequences resulting from poor sleep. (NIH authors: K.R. Dalton, V.C. Chang, M. Lee, K. Maki, V. Purandare, X. Hua, Y. Wan, C.L. Dagnall, K. Jones, B.D. Hicks, A. Hutchinson, L.M. Liao, M.H. Gail, J. Shi, R. Sinha, C.C. Abnet, S.J. London, and E. Vogtmann, PMID: 40444264)
CC, NINDS, NCI: HOPE FOR INTRACTABLE CANCER PAIN
For many battling advanced cancer, pain remains an agonizing and persistent accompaniment, often defying even the most comprehensive medical strategies. Standard treatments, reliant on opioids and anti-inflammatory drugs, frequently fall short, leaving a significant gap in effective pain management. But what if a plant-derived compound could offer a new path to relief?
Enter resiniferatoxin (RTX), a novel nonopioid analgesic found naturally in resin spurge, a cactuslike plant native to Morocco. RTX targets the transient receptor potential vanilloid 1 (TRPV1) ion channel, a key player in transmitting pain signals. When administered intrathecally, that is, into the spinal fluid, RTX selectively interrupts pain signals by affecting specific neurons, offering pain relief without compromising motor function, touch, or vital central nervous system processes such as respiration.
(Irony warning: Resiniferatoxin is a chemical analog to capsaicin, the active ingredient in chili peppers…but 15,000 times as hot as the infamous Carolina Reaper pepper. You can burn yourself just by whispering its name.)
Knowledge of resiniferatoxin’s analgesic properties dates back nearly three decades, and much work has been done in preclinical animal models and veterinary clinical pain studies examining its effectiveness. Now, in a first-in-human phase 1 trial, a team led by investigators in the NIH Clinical Center has explored the safety and efficacy of intrathecal RTX in 19 patient volunteers with refractory cancer pain—the type that does not respond adequately to standard pain management strategies.

Resiniferatoxin is a chemical analog to capsaicin, the active ingredient in peppers like the Carolina Reaper.
The findings offer a glimmer of hope. On average, these patients, with pain primarily in the abdomen or lower extremities, experienced a 38% reduction in “worst pain” intensity by the 15-day mark post-treatment, dropping from an average score of 8.4 to 5.2 on a 0–10 pain scale. Opioid consumption among participants decreased by a remarkable 57% at day 15, as well.
“The treatment was opioid sparing,” said Michael Iadarola, a senior research scientist in the CC Department of Perioperative Medicine and senior author on an interim study report published in NEJM Evidence. “The patients all voluntarily reduced their opioid consumption,” said Iadarola. “This increases alertness and their ability to participate in the activities of daily living and interact socially with family and friends.”
All 19 patients experienced some treatment-emergent adverse events (AEs), with 37 serious AEs reported in 14 patients over the 188-day study period, most being consistent with the course of their advanced cancer. Expected AEs included a temporary loss of heat sensitivity in some areas and urinary retention. Nine deaths occurred during the study, but these were attributed to cancer progression rather than the RTX treatment.
This interim study suggests that intrathecal RTX could be a valuable, single-administration, opioid-sparing option for patients with severe, intractable cancer pain, offering a much-needed alternative in the ongoing fight against suffering. RTX is a versatile interventional treatment, and the Clinical Center has also just begun a clinical trial on neuropathic pain condition called Morton’s neuroma in which RTX is injected next to the affected peripheral nerve. (NIH authors: A.J. Mannes, J.D. Heiss, A. Berger, C.C. Alewine, J.A. Butman, M.S. Hughes, N. Rabbee, C. Hayes, T.S. Williams, M.R. Sapio, and M.J. Iadarola, PMID: 40423401)
NIA, NINDS: UNTANGLING THE VIRAL LINK TO NEURODEGENERATION
Scientists have long sought to understand the connection between viral infections and brain health. Can common viruses, which can reside unnoticed within our bodies, contribute to the development of neurodegenerative diseases such as Alzheimer's and other forms of dementia? A study published in Science Advances led by researchers at the NIA tapped into data from thousands of human subjects offers compelling new insights into this enigmatic area of research.
The investigation examined the neurocognitive and plasma proteomic profiles of older adults in a community-based cohort from the Baltimore Longitudinal Study of Aging. Researchers focused on their antibody responses to four common coronaviruses and six herpesviruses with hopes of uncovering the molecular pathways linking the immune response to these viruses with brain aging and dementia risk.
The findings suggest an intriguing protective mechanism: Individuals with a more robust immune response to several common viruses, particularly the human coronavirus OC43, exhibited better neurocognitive outcomes. This level of immune robustness translated to lower odds of dementia, improved cognitive performance, and even a preservation of regional brain volumes.
How does the immune system mediate such a protective effect? The study points to a specific protein, IGDCC4 (immunoglobulin superfamily deleted in colorectal cancer subclass member 4), as a key player. Through advanced genetic analysis, the researchers demonstrated that IGDCC4 is associated with lower dementia risk over a 20-year period and causally linked to maintenance of medial temporal brain volume, crucial for memory.
This study, coordinated by NIA postdoctoral fellow Michael Duggan and NIA investigator Keenan Walker, has a strong international component that leverages data from diverse cohorts worldwide, including those from the United Kingdom, to validate its findings. This new line of research illuminates a biological basis by which our immune interactions with viruses might influence brain health in later life. Identifying IGDCC4 as an important molecular mediator not only deepens our understanding of neurodegeneration but also opens new avenues for potential therapeutic strategies targeting this protein. (NIH authors: M.R. Duggan, S.M. Drouin, D. Zweibaum, Q. Tian, J. Candia, M. Bilgel, R.F. Gottesman, L. Ferrucci, S.M. Resnick, and K.A. Walker, PMID: 40446030)

CREDIT: NIH CC
Visual representation of decision making in food selection, between ultraprocessed foods and minimally processed, whole foods.
CC: THE HIDDEN PRICE OF ACCULTURATION AND ULTRAPROCESSED FOODS
Environmental factors play a crucial role in shaping physiological changes and lifestyle, principally on dietary intake among foreign-born adults in the United States. In a recent study, NIH Clinical Center scientists found that increased consumption of ultraprocessed foods (UPFs) occurred with greater acculturation.
From the National Health and Nutrition Examination Survey (NHANES, 2011-2018), researchers retrieved data from over 3,600 non-US-born adults age 19-70. Using an acculturation index based on primary language spoken and years spent in the United States, results demonstrated that for each unit increase in acculturation, there was a 3% rise in UPF consumption.
The standard American diet (SAD) is nearly half UPFs, which include industrially processed foods that are nutritionally unbalanced and deficient, high in sugar, salt, and unhealthy fats. In line with previous findings, UPFs are related to negative health outcomes such as increased risk of cardiovascular disease, obesity, all-cause mortality, type 2 diabetes, and cancer, as well as negative metabolomic changes.
As the United States grows more diverse, eating habits give way to convenience, and health risks rise from SAD. The authors emphasized the necessity for interventions that preserve and support healthy eating habits. (NIH authors: J.J. Barb, L. Yang, A. Ahmed, P.V. Medina, E.M. Valencia, A.E. Roberts, N. Farmer, and G.R. Wallen, PMID: 40443924)
This page was last updated on Wednesday, July 9, 2025
