The 1918 Flu and COVID-19: A Tale of Two Pandemics
Anthony Fauci and Jeffery Taubenberger Launch Demystifying Medicine’s 2021 Season
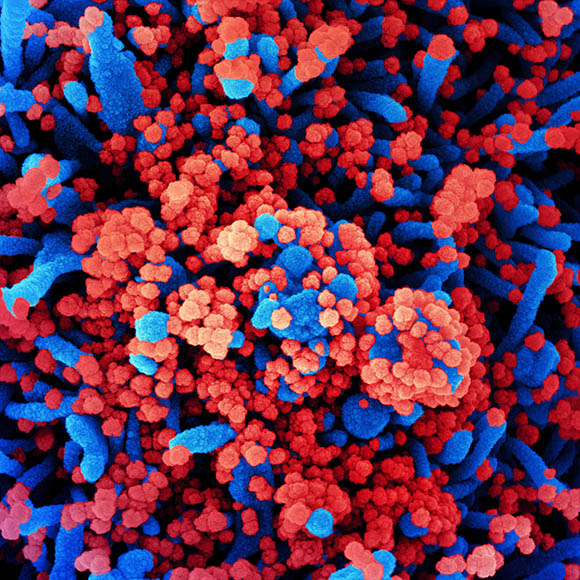
CREDIT: NIAID
Colorized scanning electron micrograph of a cell (blue) heavily infected with SARS-CoV-2 virus particles (red), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland.
The COVID-19 pandemic is not our first rodeo with battling a deadly virus, and it likely won’t be our last. As we continue to process the past year, the juxtaposition of the COVID-19 pandemic and the influenza pandemic of 1918 puts today’s challenges into perspective. Two prominent NIH scientists shared their perspectives (virtually) at the January 12, 2021, launch of the Demystifying Medicine lecture series for its 2021 season: National Institute of Allergy and Infectious Diseases (NIAID) Director Anthony Fauci and Jeffery Taubenberger, chief of NIAID’s Viral Pathogenesis and Evolution Section. Fauci gave a state-of-affairs address on what we know about the COVID-19 pandemic and what the future might hold. Taubenberger highlighted the similarities of the COVID-19 pandemic to the influenza pandemic of 1918—the pandemic that “never really went away.”
The State of Coronavirus Affairs
“We have been working with coronaviruses for decades and decades,” said Fauci. He pointed out that many are zoonotic diseases in which animals serve as intermediate hosts and viral reservoirs—such as severe acute respiratory syndrome (SARS), which went from bats to civet cats to humans in 2002, and Middle East respiratory syndrome (MERS), which went from bats to camels to humans in 2012. SARS and MERS, however, didn’t evolve into the pandemic that COVID-19, also a zoonotic disease, has.

At the Demystifying Medicine lecture on January 12, 2021, NIAID Director Anthony Fauci gave a state-of-affairs address on what we know about the COVID-19 pandemic and what the future might hold.
“We in the United States have been hit harder than any other country in the world,” said Fauci. At the end of February 2021, the United States had more than 28 million cases and over 500,000 deaths, compared with 112 million cases and about 2.5 million deaths worldwide. He painted a sobering picture of the reality of the pandemic: about 40–50% of transmissions were attributable to asymptomatic cases; older people and those with underlying medical conditions (representing 40% of Americans) are most at risk of severe disease; and racial and ethnic disparities in health-care access led to an increased incidence of infection and severity of disease among underrepresented minorities. In addition, “we are learning more and more about a very interesting phenomenon of post-acute COVID-19 syndrome,” Fauci continued. Some “individuals, after they clear the virus, have persistence for up to six months and maybe longer of lingering problems dominated by fatigue that’s profound, muscle aches, temperature dysregulation, [and] brain fog, or the inability to focus or concentrate.”
He briefly described the virology of coronaviruses, highlighting the importance of the spike proteins that sit crownlike (or corona-like) around the surface. He moved on to describing how COVID-19 is transmitted from person to person. “It’s respiratory, mainly through exposure to respiratory droplets that tend to drop within six feet,” Fauci said.
Fauci cited therapeutics such as remdesivir as well as the many COVID-19 vaccines as reasons for hope. In less than one year, we’ve gone from the availability of the genomic sequence of SARS-CoV-2, the virus that causes COVID, to the development and administration of efficacious and safe vaccines—it really was warp speed!
A Tale of Two Epidemics
Taubenberger, whose laboratory was the first to sequence the genome of the influenza virus that caused the 1918 pandemic, took us through the not-so-distant history of that cataclysmic global event.
Jeffery Taubenberger highlighted the similarities of the COVID-19 pandemic to the influenza pandemic of 1918—the pandemic that “never really went away.”
“Pandemics have happened, are happening, and will happen again,” but we’ve been caught flat-footed and found ourselves chasing this pandemic as a new coronavirus emerged in 2019, he said. In fact, our response to the 1918 pandemic was surprisingly similar, and it seems that we’re still rather “mystified” by how pandemics form, with Taubenberger pointing to a book written by a German doctor in 1820 that asked essentially the same questions we are asking today: “What is influenza? Where does it come from? How did it behave in the past? How can we predict future occurrence and halt spread?”
He also likened the world’s embrace and resistance of today’s public-health measures to those introduced in 1918—from mask wearing to school closures, as well as a moratorium on handshakes—and spitting! Despite triumphs in technology and science, this past century’s deemphasis of public-health systems have left us in an even more delicate situation than in 1918.
With 80,000 fatalities caused by influenza in 2018, are we now in a twin pandemic? As the media is consumed by the latest global coronavirus outbreak, we have heard comparatively little about this year’s flu season. One explanation for this relative lull in attention could be due to variations in influenza strains from year to year and subsequently when it might peak—we might have a later peak in 2021—and obviously our infrastructure is overburdened right now, resulting in a lack of resources for the surveillance of influenza. Taubenberger poignantly reminded us that all influenza A virus strains trace their origin to the 1918 flu—”the founder virus”—and its zoonotic jump to humans was similar to that of COVID-19. He emphasized our need to be ahead of viruses through surveillance of animal spillover events, to understand better why some viruses are more deadly than others, and to ultimately feel the urgency to develop “universal” vaccines against all viruses, not just influenza and coronaviruses.
Looking to the past for insight for our future, both scientists pointed to important lessons from past eras. Merely 100 years ago the world was devasted by the 1918 influenza, killing 675,000 people in the United States alone, equivalent to 2.5 million in today’s terms. We’ve had outbreaks before, and we’ll have them again. A universal vaccine is the way forward.
To view the videocast of the January 12, 2021, Demystifying Medicine lecture, “COVID-19 and Influenza,” go to https://videocast.nih.gov/watch=41281. For Demystifying Medicine’s full schedule and links to past lectures, go to https://demystifyingmedicine.od.nih.gov.

Eimear Holton is a social media, web, and outreach program specialist in NIAID. In her spare time, she likes to travel, practice yoga, and run road races and trails with her friends.
This page was last updated on Tuesday, February 15, 2022
