Research Briefs
CC: RESEARCHERS SEQUENCE GENOME OF A FUNGUS THAT CAUSES LIFE-THREATENING PNEUMONIA
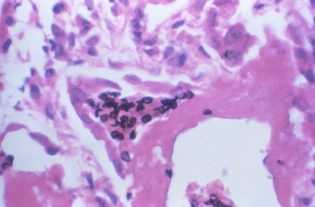
CREDIT: FRANCIS W. CHANDLER, CDC
Clinical Center researchers help sequence nearly the entire genomes of three species of Pneumocystis, a fungal pathogen that causes pneumonia and has caused thousands of deaths in immunosuppressed people such as those who’ve had transplants or are infected with HIV/AIDS. Shown here, lung tissue sample extracted from a patient ill with pulmonary pneumocystosis. The dark spots in the alveolar spaces are the fungal organisms.
Clinical Center researchers, in collaboration with scientists at Leidos Biomedical Research (Frederick, Maryland) and the Broad Institute (Cambridge, Massachusetts), have sequenced nearly the entire genomes of three species of Pneumocystis, a fungal pathogen that causes pneumonia in humans, mice, and rats. Over the past 30 years, the pathogen has caused thousands of deaths in immunosuppressed people such as those who’ve had transplants or are infected with AIDS or the human immunodeficiency virus. Efforts to combat Pneumocystis infection have been stymied by a lack of knowledge about its genome that makes it impossible to culture the organism in the lab or manipulate its DNA.
The investigators discovered that Pneumocystis is extremely well adapted to its mammalian hosts. “Our findings suggest that Pneumocystis has developed unique mechanisms of adaptation to life exclusively in mammalian hosts, including dependence on the lungs for gas and nutrients and highly efficient strategies to escape both host innate and acquired immune defenses,” the investigators wrote in their paper.
The newly acquired genomic information may lead to methods for growing Pneumocystis in the lab and allow researchers to test medications designed to kill the fungus. The information could also permit the investigators to alter the organism’s genes and determine how various genetic changes affect its ability to infect and harm its host. (NIH authors: L. Ma, G. Kutty, H. Wang, L. Bishop, E. Davey, R. Deng, X. Deng, G. Fantoni, E. Gogineni, G. Handley, C. Huber, Y. Liu, M. Sassi, X. Song, L. Walsh, Y. Xia, and J.A. Kovacs, Nat Commun 7:10740, 2016; DOI:10.1038/ncomms10740)
NIAAA: MARIJUANA-USE DISORDER IS COMMON AND OFTEN UNTREATED
In 2013, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the most recent edition, established new diagnostic criteria that combine marijuana dependence and abuse into a single disorder—marijuana-use disorder. NIAAA researchers conducted a study using the DSM-5 criteria and reported that marijuana-use disorder is common in the United States; is often associated with other substance-use disorders, behavioral problems, and disability; and often goes untreated.
The researchers applied the DSM-5 criteria to their analysis of data collected in 2012 and 2013 from a nationally representative sample of more than 36,000 American adults via the third National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III), the largest study ever conducted on the co-occurrence of alcohol use, drug use, and related psychiatric conditions. The analysis found that 2.5 percent of adults in the United States had experienced marijuana-use disorder in the past year and 6.3 percent suffered from marijuana dependence at some point in their lives. In addition, marijuana-use disorder was strongly associated with other substance-abuse and mental-health disorders, including alcohol-use disorder, major depressive disorder, and post-traumatic stress disorder. Marijuana dependence was also found to produce considerable mental disability. Finally, the study showed that only seven percent of people with past-year marijuana-use disorder and 14 percent of those who had experienced marijuana-use disorder at some point in their lives received treatment for the condition. The study authors noted the urgency of identifying and implementing effective prevention and treatment for marijuana-use disorder and the importance of educating the public about the dangers associated with marijuana use. (NIH authors: T.D. Saha, B. Huang, R. Pickering, S.M. Smith, J. Jung, H. Zhang, B.F. Grant; Am J Psychiatry DOI: 10.1176/appi.ajp.2015.15070907; NIDA contributed funding)
NICHD: PRETERM BIRTH AND AIR POLLUTION
Roughly nine percent of American women of reproductive age have asthma, according to the Centers for Disease Control and Prevention. Maternal asthma is associated with a higher risk of pregnancy complications and preterm birth (before the 37th week of pregnancy) as well as health problems for infants. In a recent study, researchers at NICHD and other institutions determined that pregnant women with asthma may be more likely to give birth prematurely when exposed to high concentrations of certain traffic-related air pollutants. Although previous studies showed that concentrations of certain air pollutants increase the risk of preterm birth, the NICHD study is the first to examine the effect of air-pollutant exposure before conception and very early in pregnancy. The researchers analyzed data from more than 223,000 single births occurring between 2002 and 2008 across the United States. They also examined daily measurements of six air pollutants in the regions surrounding the hospitals to assess the potential effects of air pollution.
The study found that higher concentrations of the traffic-related pollutants nitrogen oxides and carbon monoxide during the three months before conception and the first seven weeks of pregnancy increased the incidence of preterm births more in mothers with asthma than those without. Increased exposure to small particulate matter late in pregnancy had the same effect. The researchers hope their findings will prompt additional studies aimed at reducing the risk of preterm births in women with asthma. (NIH authors: P. Mendola, M. Wallace, B.S. Hwang, D. Liu, R. Sundaram, and K.L. Grantz, J Allergy Clin Immunol DOI:10.1016/j.jaci.2015.12.1309)
NINDS: EXPERIMENTS SUGGEST NMDA RECEPTORS HELP THE BRAIN DETECT MOTION
A series of experiments performed by NINDS scientists suggest that a protein called the N-methyl-D-aspartate (NMDA) receptor helps neurons in the eye and brain filter out background noise to detect movement. NMDA receptors have long been associated with learning and memory but have never before been linked to motion perception.
The researchers passed bars of light across retinas isolated from mice and recorded the electrical responses from neurons called directionally selective retinal ganglion cells (DSGCs), which are activated by stimuli moving in specific directions. By exposing the DSGCs to moving bars of light set against backgrounds of varying brightness, the NINDS team discovered that NMDA receptors helped the neurons send consistent signals about the direction of each bar’s motion despite variations in the level of background light. The NMDA receptors did this by amplifying the cells’ responses to the bars via a process called multiplicative scaling.
The results shed light on how neurons distinguish useful information in the visual environment from irrelevant inputs. The researchers now hope to examine whether NMDA receptors play a role in other visual processes as well. (NIH authors: A. Poleg-Polsky and J.S. Diamond, Neuron 89:1277–1290, 2016)
NIAID: FACTORS THAT MAY INFLUENCE INFLUENZA VACCINE EFFECTIVENESS
The system for predicting the effectiveness of the seasonal flu vaccine may need to be changed, according to a study conducted by NIAID researchers. Currently, seasonal flu vaccines are designed to induce high concentrations of protective antibodies against hemagglutinin (HA), a protein found on the surface of the influenza virus that enables the virus to enter a human cell and initiate infection. However, wide variations in the effectiveness of recent vaccines prompted the researchers to examine whether other factors should be considered.
The researchers conducted a clinical trial—called a human challenge study—in which 65 healthy volunteers (aged 18 to 50 years) were exposed to naturally occurring 2009 H1N1 influenza type A virus and monitored for eight weeks. The flu challenge study, which began in September 2013, was conducted at the NIH Clinical Center in the specially designed Clinical Studies Unit, which has distinct isolation and infection-control features. The researchers found that higher concentrations of antibody against a different flu surface protein—neuraminidase (NA)—were a better predictor of protection against flu infection and its unpleasant side effects. NA, which is not currently the main target antigen in traditional flu vaccines, enables newly formed flu viruses to exit the host cell and cause further viral replication in the body.
Participants who had high concentrations of HA antibodies were considerably less likely to develop mild-to-moderate influenza during the eight-week period and also fought off the illness more quickly than those with lower concentrations of HA antibodies. However, both groups experienced roughly the same number and severity of flu symptoms. On the other hand, those with high concentrations of NA antibodies were not only less likely to get sick but also experienced symptoms that were less numerous, less severe, and briefer than those with low NA antibody concentrations or high HA antibody concentrations. Participants with high concentrations of both types of antibodies were the most protected against the virus. The findings suggest that NA antibodies may be a better predictor of influenza immunity than HA antibodies and should be taken into account when attempting to estimate the efficacy of future vaccines. (NIH authors: M.J. Memoli, A. Han, L. Czajkowski, S. Reed, R. Athota, T. Bristol, S. Fargis, K. Risos, J.H. Powers, R.T. Davey, Jr., and J.K. Taubenberger, mBio 7:e00417-16, 2016; DOI:10.1128/mBio.00417-16)
NIDCR: IDENTIFICATION OF IMMUNE CELLS IN HEALTHY MOUTH LAYS GROUNDWORK FOR UNDERSTANDING PERIODONTAL DISEASE
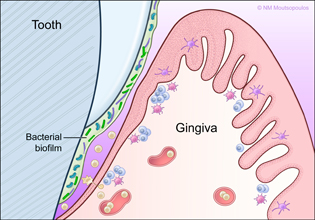
CREDIT: NIKI MOUTSOPOULOS, NIDCR
Immune defense of the gingiva (soft tissue surrounding the teeth) is important because they lie close to the bacterial biofilms that coat the surface of teeth.
NIDCR and University of Manchester (Manchester, England) researchers have identified the immune cells that reside in the gingival tissues surrounding the teeth, a key barrier site. Defending this soft tissue barrier is especially important because it is continually exposed to commensal bacterial biofilms, which adhere to the teeth. This study is the first detailed immunophenotyping of human oral tissues and provides a foundation toward the characterization of the oral immune system in health.
The analysis revealed a predominance of T cells and neutrophils in healthy gingival tissues as well as a sophisticated network of antigen-presenting cells. The researchers also noticed a small population of innate lymphoid cells, a recently described type of cell not previously known to inhabit human gingiva. When the team examined similar biopsies from a small group of people with periodontitis, it saw elevated numbers of neutrophils and increased concentrations of the cytokine interleukin-17 (IL-17). Although neutrophils and IL-17 are part of the host’s defense, they have the potential to contribute to damaging inflammation if overproduced.
By painting a detailed picture of the immune-cell landscape under normal circumstances, the findings represent a baseline that scientists can use to track changes that occur under disease conditions. Ultimately, this information provides the foundation for identifying drug targets and developing novel strategies for treating diseases of the oral cavity. (NIDCR authors: N. Dutzan, T. Greenwell-Wild, and N. Moutsopoulos, Mucosal Immunol DOI:10.1038/mi.2015.136; link: http://www.ncbi.nlm.nih.gov/pubmed/26732676)
NIAID, FDA: EXPERIMENTAL DENGUE VACCINE PROTECTS RECIPIENTS IN VIRUS-CHALLENGE STUDY
A recent clinical trial showed that a dengue virus vaccine, developed by researchers at the NIAID with help from FDA’s Center for Biologics Evaluation and Research, provided complete protection against the virus. Dengue fever is spread by mosquitoes of the genus Aedes, the same one that carries the Zika virus, and infects approximately 390 million people each year, mostly in tropical and subtropical regions. Although most infections produce only mild symptoms or none at all, some cause more serious illness that can be life-threatening. Unfortunately, the vaccine candidate currently furthest along in clinical trials has proven only sporadically effective.
Because individuals previously infected with dengue fever may develop immunity to some forms of the virus, it can be difficult to measure the efficacy of potential vaccines in areas where the virus is prevalent. Consequently, the researchers performed a human challenge study in which 41 healthy American adults were given the vaccine or a placebo and then exposed six months later to a modified version of the dengue virus designed to cause only mild illness.
After virus exposure, all 20 of the volunteers given the placebo developed infection. The 21 individuals who received the vaccine, called TV003, did not. The results have prompted Brazilian researchers to undertake a large phase 3 clinical trial in regions where dengue fever is commonly found, an important step given that such studies are the gold standard for determining the efficacy of vaccines. Moreover, variations of the modified dengue virus used in the NIAID study may help researchers test the effectiveness of other dengue vaccines. Finally, because dengue virus is related to the Zika virus, the dengue vaccine study may help researchers develop a Zika vaccine. (NIH authors: S.S. Whitehead, Sci Transl Med 8:330ra36, 2016)
This page was last updated on Wednesday, April 13, 2022
