Precision Psychiatry
Research Domain Criteria Leading the Way
Imagine you arrived at a hospital emergency room before the advent of modern medicine with intense abdominal pain. You could have had a stomach virus, kidney stones, appendicitis, or something worse. But because the doctors lacked the proper diagnostic tools and knowledge to identify your illness, the only thing they could do was treat your most prominent symptom—your pain.
For many with mental-health problems this scenario is still close to reality. There are no lab tests to diagnose what’s wrong, so clinicians have no choice but to treat the symptoms—such as hallucinations in schizophrenia—but not the underlying disorder. And, like abdominal pain, each of the symptom-based diagnostic categories may include a diverse group of disorders.
Until recently, most mental-health diagnoses, treatments, and research have been structured according to definitions in the Diagnostic and Statistical Manual of Mental Disorders (DSM). The DSM, which was first published in 1952 and has been continuously revised and improved since then, uses clusters of symptoms agreed upon by psychiatrists to classify disorders into such categories as major-depressive disorder, autism, and schizophrenia. Although the manual is useful in that it provides a consistent terminology, it lacks the precision that derives from objective biological, behavioral, and socio-cultural information.
In an attempt at precision medicine for psychiatry, the National Institute of Mental Health (NIMH) launched the Research Domain Criteria (RDoC) initiative in 2009. RDoC provides a research framework for classifying mental disorders based on many kinds of objective measures instead of according to the traditional subjectively-based DSM groupings.
Despite decades of research, scientists have been unable to find any genetic or neurological evidence to support the breakdown of the disorders into the DSM categories. So far, no cellular or genetic signatures for any mental disorder have been discovered, nor has anyone developed reliable biomarkers, blood tests, or brain scans that match perfectly with a DSM-defined mental illness. NIMH is betting that the problem is the diagnostic system and that focusing on the biomarkers may provide diagnostic categories more useful for selecting treatments and improving outcomes. Because the focus of the field has been solely on understanding mental disorders as defined by the clusters of symptoms in the DSM, most current treatments have aimed at relieving symptoms rather than resolving the underlying pathology.

“Our diagnostics are limited to symptoms clusters; we need the powerful tools of genomics and neuroscience for more precise diagnostics and better treatments,” explained NIMH Director Thomas Insel.
“Our diagnostics are limited to symptom clusters; we need the powerful tools of genomics and neuroscience for more precise diagnostics and better treatments,” explained NIMH Director Thomas Insel. “We can reduce hallucinations, but we are not treating schizophrenia. We can relieve symptoms of depression, but that may not be treating the underlying disorder.”
RDoC is already changing the way mental-health researchers approach the study of mental disorders.
“RDoC is about translating basic research into an understanding of psychopathology,” explained NIMH clinical psychologist Bruce Cuthbert, who heads the RDoC project and runs educational webinars, workshops, and a forum for researchers to discuss RDoC issues. “What did the brain normally evolve to do? How does it do it? What goes wrong in these circuits [and] systems?”
Using the RDoC approach, scientists are trying to better understand mental illness by focusing on the convergence of biology and behavior and tying different aspects of behavioral, cognitive, and emotional functions to specific brain systems. The research is organized into five broad domains: positive valence (seeking and appreciating reward), negative valence (threat and loss), cognitive systems, social systems, and arousal and regulatory systems.

“RDoC is about translating basic research into an understanding of psychopathology,” explained NIMH clinical psychologist and RDoC project head Bruce Cuthbert.
Some scientists are relying on an RDoC approach to investigate the biological underpinnings of anhedonia, the inability to seek or experience pleasure in normally pleasurable activities such as exercise, sex, and socializing. Anhedonia occurs in a variety of DSM-defined disorders—including depression, bipolar disorder, certain anxiety and personality disorders, and schizophrenia—yet there are no FDA-approved treatments for it.
NIMH senior investigator Carlos Zarate, who is interested in developing novel medications for treatment-resistant depression and bipolar disorder, has linked anhedonia to changes in brain activity. In one trial, his team administered ketamine to patients with bipolar disorder. Ketamine produces a rapid antidepressant effect within hours and lasts less than a week. But, surprisingly, the team found that it had an even an more powerful effect on anhedonia: Within 40 minutes of receiving ketamine, patients experienced a sharp reversal in anhedonia—and the effect lasted up to 14 days.
To determine which area of the brain was affected, Zarate’s group used a brain-imaging technique called positron-emission tomography (PET). Earlier research that measured ketamine’s antidepressant effects showed changes in the ventral striatum, a brain area linked to reward-seeking behavior. But when measuring changes in the hedonic drive, Zarate found that ketamine affected another area of the brain—the dorsal anterior cingulate cortex, a region involved in reward processing, learning, and decision-making. The results were observed in patients who had bipolar disorder (a type of depression in which there are low moods as well as high moods and activity levels, or mania) and those with unipolar depression.
In related research, Zarate is trying to link anhedonia to changes in brain function in relation to attempted suicide. Suicide has been a relatively neglected area of mental-health research, according to Insel. “This year there will be more deaths from suicide, almost all related to mental illness, than from breast cancer or HIV or homicides,” he said. “It’s just phenomenal how great the morbidity and mortality is. It goes unrecognized.”

PHOTO BY RHODA BAER
Carlos Zarate uses PET imaging techniques to measure changes in how the infusion of ketamine affects brain activity in patients with treatment-resistant major depression.
Anhedonia plays a role in suicidal thoughts, according to Zarate, and ketamine can reverse them. “We’ll be studying people with current suicidal thoughts irrespective of DSM diagnosis. Such participants may have prominent depression or not, or may primarily have an anxiety disorder or may not even have other prominent psychiatric symptoms as in the case of someone who has lost all their money in the stock market,” said Zarate. “That way we will look at the biology of suicidal thoughts across psychiatric disorders.” Because there is very little known about the brain circuits implicated in suicidal thoughts, Zarate and his team are planning to use multi-modal neuroimaging techniques to map brain areas involved with ideation (the process of coming up with new ideas) and to probe ketamine’s rapid antisuicidal effects.
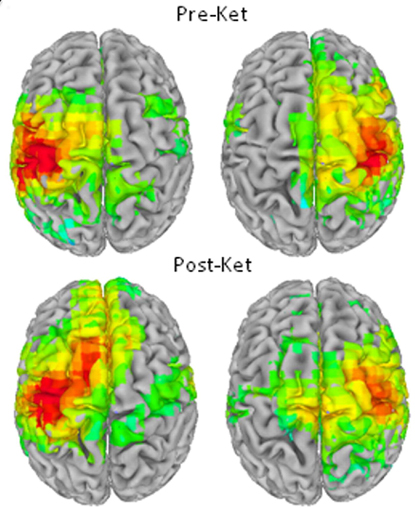
Brain images :(above) brain before ketamine infusion; (below) after the infusion of ketamine, different areas of the brain become activated.
Anhedonia is also being studied by extramural researchers including former NIMH scientist Jerzy Bodurka, now at the Laureate Institute for Brain Research (Tulsa, Oklahoma). He is analyzing gene expression and using advanced imaging techniques to study how inflammatory cytokines may trigger dysfunction in brain circuits that control motivation and pleasure. In theory, if mechanisms of anhedonia could be identified, patients could be tested for them and treated, whether or not they have a DSM diagnosis.
NIMH senior investigator Daniel Pine uses the RDoC framework to investigate a process known as fear extinction, or the ability to deliberately ignore fear. He uses functional magnetic resonance imaging to study the connection between the basal lateral amygdala and ventromedial prefrontal cortex, a brain circuit involved in the ability to forget fearful memories. He believes that dysfunction of this circuit may occur in children who have problems with stress and anxiety.

Daniel Pine uses functional magnetic resonance imaging of the brain to determine whether a dysfunction in a particular brain circuit plays a role in children who have problems with stress and anxiety.
Another NIMH senior investigator, Ellen Leibenluft, is also being guided by the RDoC approach as she uses imaging techniques to investigate brain mechanisms that mediate bipolar disorder and severe irritability in children and adolescents. “Irritability fits well as an RDoC construct,” she explained. “It’s dimensional—some people are pretty chill, others very irritable—and it cuts across many diagnoses: Children with anxiety, attention-deficit hyperactivity disorder, autism, [and] depression are irritable.” Had she been guided solely by the DSM, she might have been looking at brain activity in association with a diagnosis. Instead, she’s looking at how irritability affects the brain.
Ellen Leibenluft is also being guided by the RDoC approach as she uses imaging techniques to investigate brain mechanisms that mediate bipolar disorder and severe irritability in children and adolescents.
The RDoC was originally designed in the hope that researching mental diseases by dimensions—such as irritability, anhedonia, fear extinction, and other behaviors—instead of by symptom-organized diagnoses would generate a biological definition for mental disorders, and that in turn will facilitate the discovery of new treatments that target the underlying pathology.
“It will give us much better guidance about what treatments should be given to which people,” said Insel. “It really is precision medicine for psychiatry.”
To learn more about RDoC, go to http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml.
This page was last updated on Monday, April 25, 2022
